Between five to 12 women out of 10,000 are at risk of developing a blood clot while on the contraceptive pill, according to The European Medicines Agency. Press and Journal social media manager Katie Forbes was one of those unlucky few.
Katie went from being a fit triathlete who thrived on swimming, cycling and running upwards of 100km each week, to being overwhelmed with exhaustion from merely climbing a flight of stairs.
The 26-year-old assumed she was suffering with some kind of bug, but little did she know, she was in fact experiencing the symptoms of a potentially life-threatening pulmonary embolism (blood clots in her lung).
Millions of women take the contraceptive pill every day – many of whom are often unaware of the potential risks.
While the NHS say the risks are low, Katie wants to share her story to help educate people on the signs, symptoms and red flags associated with developing a blood clot.
Never did I expect as a young triathlete that I would be left gasping for air from simply talking.
Yet, here I was, in morning news conference struggling to get my words out, as if I had just finished a triathlon. My chest pounding as my heart raced and coughs threatened to escape.
I laughed it off, eager to continue working, but alarm bells were ringing in my ears.
My friends and I consulted Dr Google and began guessing what may be wrong – anxiety, chest infection and so on… but no one suspected anything life-threatening.
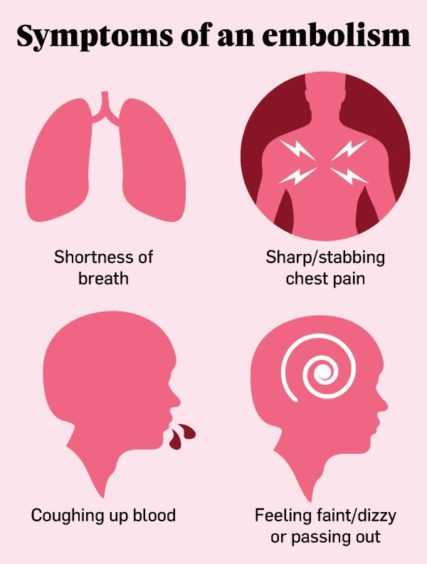
I had started experiencing shortness of breath four weeks prior, during a gentle run.
On a route I’ve taken countless times over the last seven years, I found myself panting on the slightest of inclines.
I laughed it off initially – typical Aberdonian, finding 18 degrees too hot to handle!
But when this continued and new symptoms surfaced – rapid heartbeat, back pain, and excessive sweating – I carried out Covid tests (all of which came back negative), then decided to get in touch with my GP.
‘There was an invisible barrier holding me back’
I spoke to a doctor the following day, but he wasn’t concerned and asked me to get back in touch only if my symptoms persisted or worsened.
Over the next two weeks, being stubborn as I am, I continued triathlon training. However, there was an invisible barrier holding me back.
The only thing getting quicker was my heart rate, and although I wasn’t fevered, I was overheating and felt light-headed.
Soon I was breathless even at rest. I was forced to stop exercising.
I submitted another econsult with my doctor and yet again my request wasn’t met with urgency. I didn’t receive a response for two days.
Finally, three days after submitting the econsult, and now experiencing chest pain, I was sitting across from my doctor relaying the eventful last few weeks.
She admitted she was stumped, so I underwent an examination, ECG and many blood tests. One hour later, I was on my way to Aberdeen Royal Infirmary.
‘(The blood clot) was now large enough to put strain on my heart’
I was admitted immediately to Ward 101, before I was yet again poked and prodded by needles and the subject of various tests and scans.
My resting heart rate – which typically sat between 40-50bpm – caused alarm at 120bmp. My temperature spiked and my chest pain intensified.
The pain started encroaching on other areas, too. A continuous dull ache was now present in my right shoulder, arm and side, and a sharp pain struck every time I took a breath.
Despite the numerous nurses and support workers whizzing around me, I felt terribly alone.
My husband could attend a football game at Pittodrie alongside 19,000 other people, but he wasn’t allowed into my room, containing three people.
Although I understand hospitals need to be cautious, only having my anxious thoughts as company was unsettling – and certainly didn’t help my rapid heart rate.
Later, my chest x-ray and CT scan showed I had extensive bilateral pulmonary emboli – several blood clots in my lungs and a rather large clot in my right.
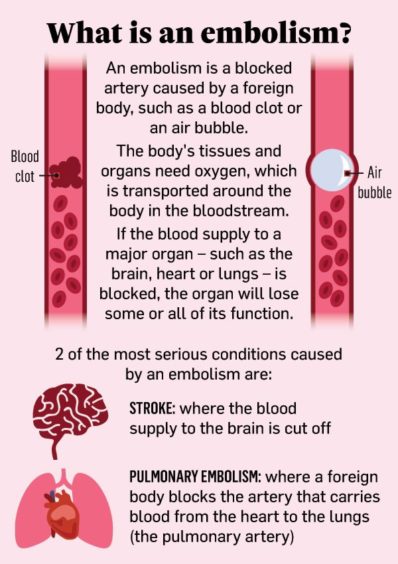
The large clot, which the doctors believed had grown gradually over time, was now large enough to put strain on my heart, causing my breathlessness and pain.
‘I jolted awake with unimaginable pain’
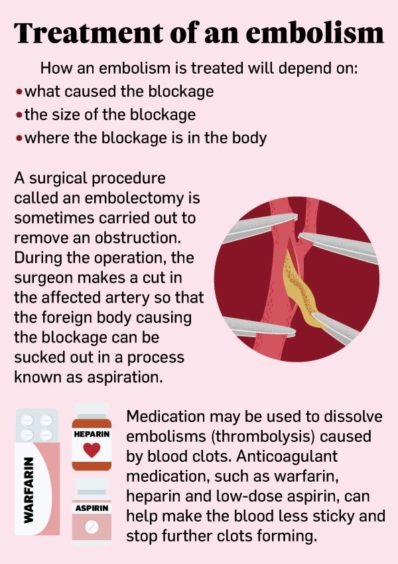
I was started on a course of blood thinners to increase blood flow and help prevent clot growth, as well as pain relief.
The doctors insisted I stay in the hospital for the next 24 hours for observation as I started my treatment. I was moved upstairs to ward 103 (the short stay medical ward), and was thankful to have my own private room.
Support workers and nurses welcomed me to the ward. Their kindness and dedication always brought a smile to my face, no matter how much pain I was in – and some even managed to evoke laughter.
I sobbed into my mask, with every gulp of air sending electric shocks to my chest and side.
They started my blood thinners course with a nippy injection, that bruised both my stomach and ego, and I was prescribed paracetamol and Dihydrocodeine – an opioid given for relief of moderate to severe pain. I then settled for an early night.
At 4am, I jolted awake with unimaginable pain spearing across my chest to my right side and arm.
A doctor promptly arrived to examine me, before prescribing oramorph, liquid morphine that is taken by mouth.
An hour past and I was now crying out in pain. As a nurse practitioner examined me, I sobbed into my mask, with every gulp of air sending electric shocks to my chest and side.
Another dose of oromorph was administered, leaving a sweet yet bitter taste in my mouth. The pain was unbearable unless I laid on my left side, so that’s how I stayed for the remainder of the night.
‘Just like that, my life was altered in an instance’
I was discharged that afternoon with my very own pharmacy to bring away with me. I would return to the hospital in three months to repeat scans and have an echogram, to ensure there was no long-lasting damage to my heart or lungs.
The chest pain would subside within one week, but I would remain breathless for up to six weeks – not to mention the months of rebuilding my strength thereafter.
And just like that, my life was altered in an instance.
‘The risk of blood clots is often brushed over when talking about the combined pill’
My fast-paced, thrill-a-minute job, my evenings and weekends of swimming, cycling and running alongside friends, fun wine-filled date nights with my husband – the things I filled my life with, that made me, me, were all in jeopardy.
All because of a tiny, seemingly harmless pill. The risk of blood clots is often brushed over when talking about the combined pill.
Some downplay it as a “side effect” – or fail to mention it at all during contraception consultations. Yet, this “side effect” could be fatal.
Like many of my peers, I started the pill in my teens, as many are led to believed it is the solution to acne and irregular periods.
When I visited my GP to discuss contraception, this seemed to be their preferred method.
They quickly brushed over the possible side effects, but not once during the initial consultation, or the near eight years that followed, did they highlight the red flags I should be looking out for.
Now, as I’m high risk to blood clots, I’m no longer allowed to take the combined contraceptive pill. However, doctors have advised I am able to take the progesterone-only (mini) pill, which apparently doesn’t have the same risks.
But when my symptoms first appeared, not I, my friends – or GP for that matter – suspected it was a clot.
If I had not called the doctors and insisted on being seen when I did, I may not have been here to write this.




