Aberdeen University researchers have warned doctors that handing out opioid painkiller prescriptions to patients on hip and knee operation waiting lists could be doing more harm than good.
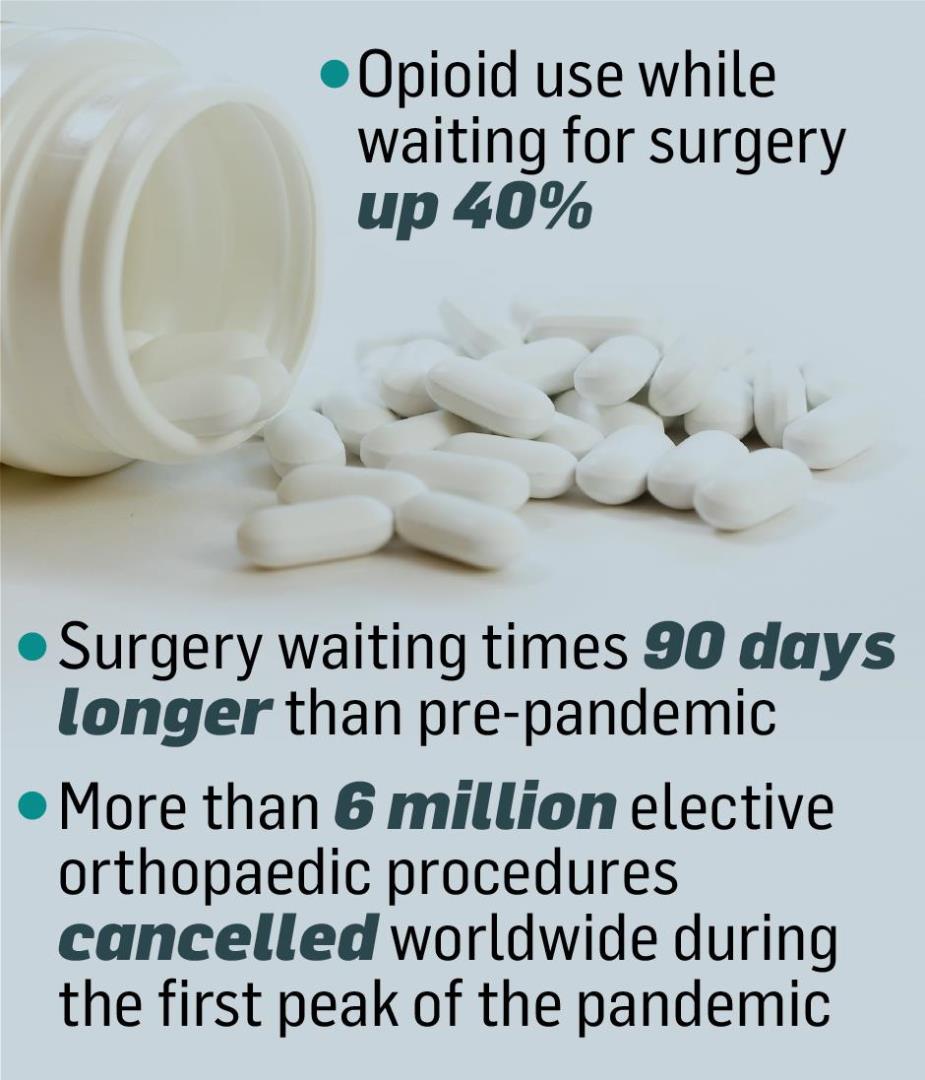
A new study, published today in the BMJ Quality & Safety, has found there are 40% more patients waiting for an operation and taking opioids for pain relief compared to pre-pandemic levels.
Opioids – painkilers derived from opium, such as morphine and tramadol – are often used as a last resort in pain management for osteoarthritis.
But there is growing evidence to suggest they are not as beneficial as first thought, and could even harm people’s health in the long-term, especially for older adults.
Surge in opioid use linked to waiting time for surgery
The researchers said the long-term use of opioids before surgery can be linked to an increased risk of complications during the operation, poorer outcomes and ongoing opioid dependence.
The surge in opioid use identified was associated with overall waiting times for surgery, which have been, on average, 90 days longer during the pandemic.

Hospitals worldwide were forced to restructure when the pandemic hit, as they to make an immediate shift towards prioritising acute and emergency care.
This led to the widespread delay of elective orthopaedic procedures.
Patients awaiting hip and knee replacements, as one of the most common elective procedures, have been disproportionally affected.
Estimates suggest more than six million elective patients had their procedures cancelled worldwide during the first peak of the Covid pandemic.
Pandemic impacted access to hip and knee surgery
Luke Farrow, a clinical research fellow at Aberdeen University’s Institute of Applied Health Sciences which led the project, said: “While these changes have served to ‘flatten the curve’ and reduce some of the harm associated with Covid-19 infection, there has undoubtedly been an impact on patients.
“Covid-19 has had a significant detrimental effect on access to hip and knee surgery.
“Work by others has suggested this has been associated with worsening pain and quality of life for patients.”
‘Avoid the use of opioids if at all possible’
The study centred around data from 452 north-east NHS patients who were on the waiting list for hip and knee replacement surgery.
Researchers compared the number of those waiting who had been prescribed opioids with those who had surgery before the pandemic.
Luke added: “Our work provides evidence of potential for an emerging opioid problem associated with the influence of Covid-19 on elective orthopaedic services.
“With continued delays (for) total hip and knee arthroplasty expected for some time, due to the considerable backlog… patients will need to seek alternative treatment options to manage their symptoms.

“We would advocate that healthcare professionals and patients avoid the use of opioid medication if at all possible due to the known lack of effect in this setting and potential for harm.
“We urgently need to find better alternative methods for managing severe arthritis pain for those awaiting this type of surgery and work to recover the backlog… to prevent to prevent more widespread opioid use.”
