Cervical cancer is the most common cancer in women under the age of 35 in Scotland.
Almost all cervical cancer cases are linked to human papillomaviruses (HPV) – a group of viruses that most people will eventually come into contact with in their lives.
The virus is usually harmless with the infection normally going away by itself and most people never even know they’ve had it.
But in some cases it can turn into genital warts, or even cancer.
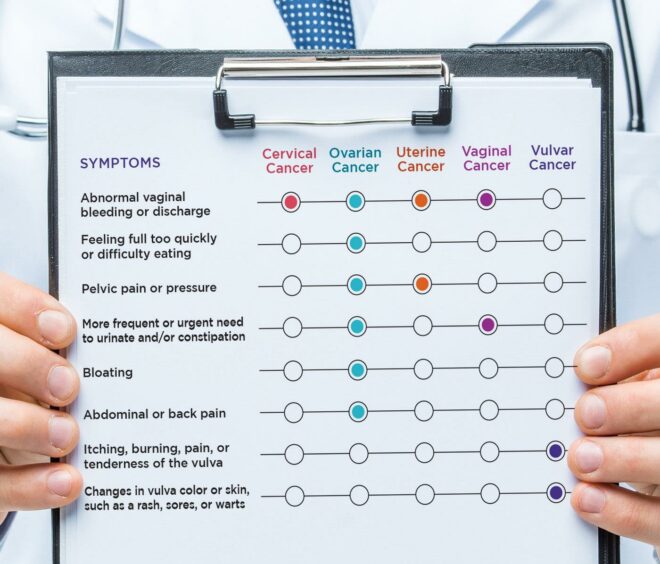
There are five different gynaecological cancers – cervical, vulval, vaginal, ovarian and womb – and HPV can cause the first three types.
What are the symptoms of gynaecological cancers?
September is National Gynaecological Cancer Awareness Month, a time dedicated to
raising awareness of the symptoms of female reproductive system disease.
Every year, over 21,000 women are diagnosed with a gynaecological cancer, and approximately 99.8% of cases are preventable.
And while there are many different symptoms, these are the most common signs to look out for:
- Unusual bleeding between periods
- Vaginal discharge
- Pelvic pain
- Vaginal lumps or growths
How can we avoid infections turning into cancer?
It is important for women to go for their smear tests at their local GP surgery.
Test samples are checked for the type of HPV which can cause changes to the cells of your cervix.
Any changes discovered can be treated before they turn into cervical cancer.
A vaccine is also available to help prevent HPV infections which helps protect the immune system.
Children aged 12 or 13 can get the vaccine through the NHS and it is usually given at schools.
Men who have sex with men are also at higher risk and can get access to the vaccine at sexual health clinics.
The vaccine is also available privately and you can get more information on this from your GP.
Reducing the number of sexual partners you have will also cut down the risk, as well as ensuring you have protected sex.
We need to reduce the stigma attached to HPV
Healthcare tech company myGP highlights that sexual health awareness is still a taboo in our society with most people avoiding the topic.
Their medics say referring to HPV as a sexually transmitted infection spreads misconceptions about the virus which could lead to internalised negative feelings.
“While HPV and sexually transmitted infections share some similarities, most of us will have HPV regardless of sexual behaviour,” a spokesman said.
“Therefore, the level of stigma associated with the virus needs to change. Women need to be empowered to understand HPV properly and to feel comfortable getting their bodies checked.
“Health is a precious thing, let’s not take it for granted and keep on top of our tests and examinations.”
More health news…
Catch up on the first article of our new wellbeing series exploring why low carb diets are dangerous
Struggle with Sunday night dread? Here’s how to cope with it