NHS Grampian bosses fear this winter will be their toughest yet, and have revealed patients are experiencing a “merry-go-round of pain, distress, upset and frustration”.
After 18 months of the pandemic, health board chiefs say staff are at breaking point and a £10m post-Covid black hole is looming.
Cancer treatment rates have plummeted to the lowest level in Scotland, while more than 2,000 patients requiring the most serious treatments are stuck on waiting lists.
And on one day last month, just 39 of the 670 total beds were available at Aberdeen Royal Infirmary, with some wards completely full.
But NHS Grampian chief executive Caroline Hiscox has stressed there are plans in place to cope with a winter surge, building on the experiences of Covid so far.
Thousands left on waiting lists
Reports going before the NHS Grampian board today outline the plan for Operation Iris, the latest strategy for coping with the pandemic.
It comes after operations Rainbow and Snowdrop, named on the advice of army majors assisting the board’s pandemic planning.
The documents state the pressure on healthcare is apparent “in all areas”, with shocking figures laying bare just how bleak the situation is.
A snapshot of data shows wards at Aberdeen Royal Infirmary were at 94% capacity on November 19.
Of the 50 critical care beds within the hospital, just five were available.
That day a total of 66 patients were being treated for Covid, while a further five had suspected coronavirus. At one point last month, ARI was treating the most coronavirus patients time since January.
Meanwhile the waiting list for inpatient procedures – including the likes urology, general surgery and gynaecology – grew even further, to almost 18,000.
Of these, close to 12,000 had been waiting more than 12 weeks to be seen. One-fifth, or 3,700, had been waiting more than 78 weeks.
‘Discomfort’ ahead
Bosses say it is “likely” that some patients will not experience the same level of care they would have received pre-pandemic.
“Perhaps more commonly [experienced],” the documents stated, “Will be the discomfort, inconvenience and worry associated with longer waiting times.”
Part of this is due to the enhanced infection control measures, and lowered staff-to-patient ratios on the wards.
Bosses said: “This will undoubtedly increase the risk of a reduction in the quality of care.
“However, this is a risk being considered against providing no care for others if we do not expand the system to meet the pressure.”
Patients tell of ‘mental anguish’
The documents include harrowing stories from some anonymous patients categorised as “low priority” and waiting for treatments.
One said: “The mental anguish during the wait for surgery is something I had never expected to feel.
“It’s hard enough finding out there is something wrong with your body, but learning that you have to wait for an unknown amount of time to get it fixed is unbearable.
“I’ve found myself on edge with anxiety, enduring many sleepless nights”.
Another said the wait had turned life into “a merry-go-round of pain, distress, upset and frustration.”

A third patient said: “I don’t know what to do any more. I can’t afford to live without working.
“I can’t cope with the pain much longer. No one really cares enough to do anything.
“I’ve been keeping my chin up and staying positive for the outside world for 26 months now to keep everyone else happy but I’ve had enough now. I just don’t want to do it any longer.”
NHS Grampian in ‘strong position’ for winter
Prof Hiscox said the board papers highlight how NHS Grampian is being “realistic and transparent” about the pressures it is facing.
But she also hopes they can instil some public confidence as we head into winter.
“Actually we’re in the strongest position to continue to lead through the next six months,” she said.
“We are well practised now, living and working with this pandemic, and can manage in a very different way things that are presented to us at a quick pace.
“This is possibly going to be the most challenging winter we as a healthcare system have faced, but we have 20 months now of learning about how to do this.
“Our system remains very constrained [and] access for patients is nowhere near where we would like it to be.
“We are prioritising access, and making sure that how we do that is risk assessed.”
‘No simple fixes’ for the future
Today the board will discuss new procedures to help manage day-to-day operations, and the way forward for when additional Covid funding comes to a close.
Since the start of the pandemic, more than 1,000 new staff members have been recruited with hundreds more joining the workforce over the coming months – at a cost of around £10m.
And the papers admit there are no “simple fixes” to the situation, with a need to completely overhaul the health and care system.
“Despite all the innovations, the way we are currently delivering our services means we are unable to keep up with the growing demand,” the documents said.
And this need for change has been echoed by others involved in the healthcare system.
Martin McKay from the Grampian branch of trade union Unison said: “It’s a complex situation we’re in and there’s no easy solution.
“But we can’t expect staff to give more with less. Sometimes hard decisions need to be taken.
“Everyone is expecting to go back to normal but we’re nowhere near that.”
Solution could be years away
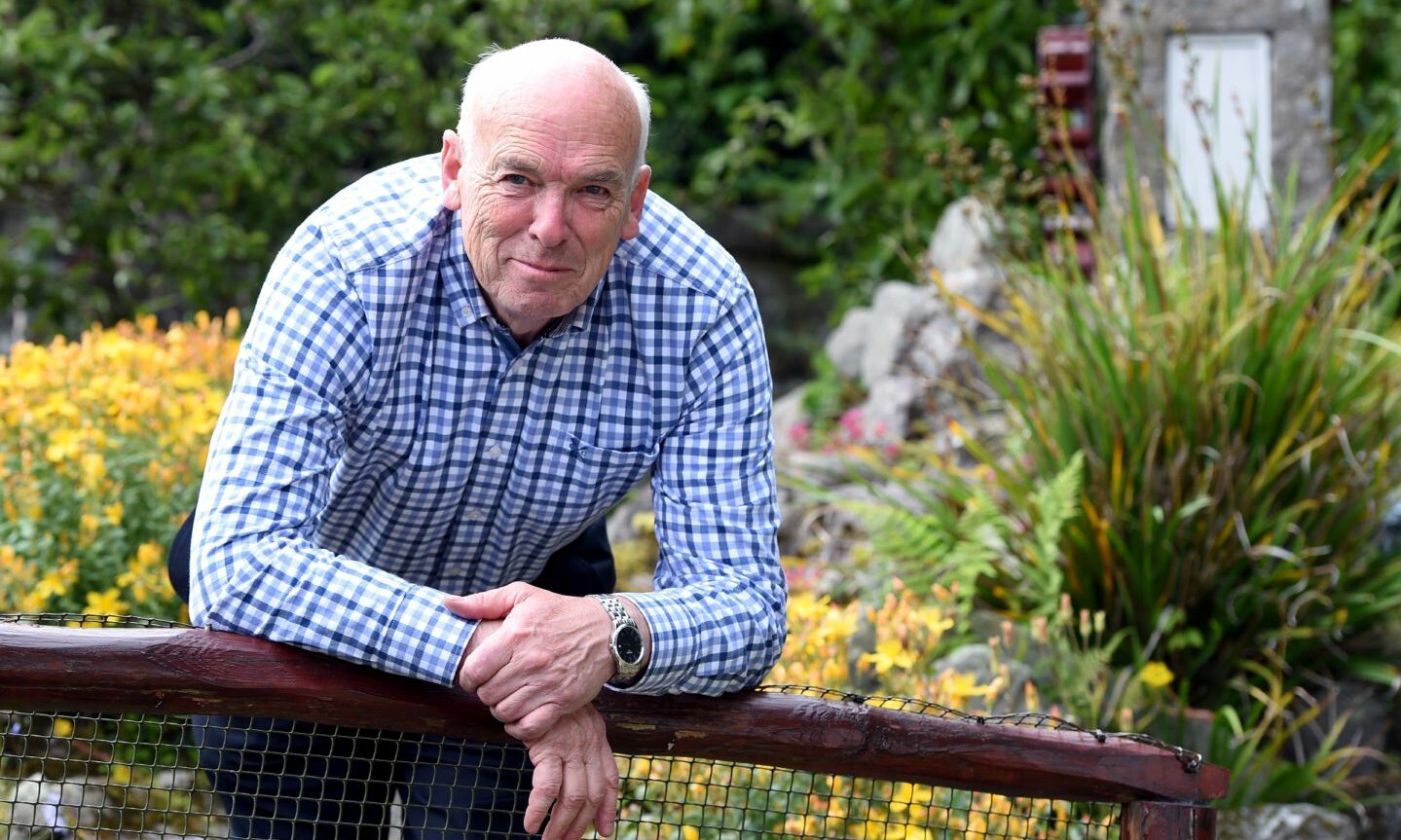
Jamie Weir, spokesman for the patient group PACT, said the NHS was already under “intense pressure” before the pandemic.
He fears it could be “many years” before the system is able to function at a sustainable level once more.
And while he knows NHS Grampians is doing “its very best,” Prof Weir says a “major rethink” is required to move forward.
“For patients to be reassured that their needs are met, at the appropriate times, with staff fully trained and not exhausted, is going to require a long term plan that will need considerable resource,” he added.
“It is up the politicians to develop such a plan and not merely to throw money at various health boards to try and achieve short term fixes which are not working.
“It takes many years of training for doctors, nurses, paramedics and many other healthcare workers and any plan has to include these factors.
“There is not a ready pool of people to fill even the current posts – let alone increasing the services needed and desired by patients.”