Health bosses have painted a stark picture of NHS Grampian, revealing a growing financial black hole, soaring ambulance wait times and ward safety concerns.
The health authority’s board will meet today to discuss a range of factors, including some of the key statistics used to measure performance.
It says “significant” work is underway to remedy these, but more problems are emerging to put even more strain on the system.
By the end of August, NHS Grampian had already recorded a £17 million deficit – nearly twice what it previously predicted.
This is only adding to the immense pressure the health board is already facing – laid bare in a report using figures for the week to September 13.
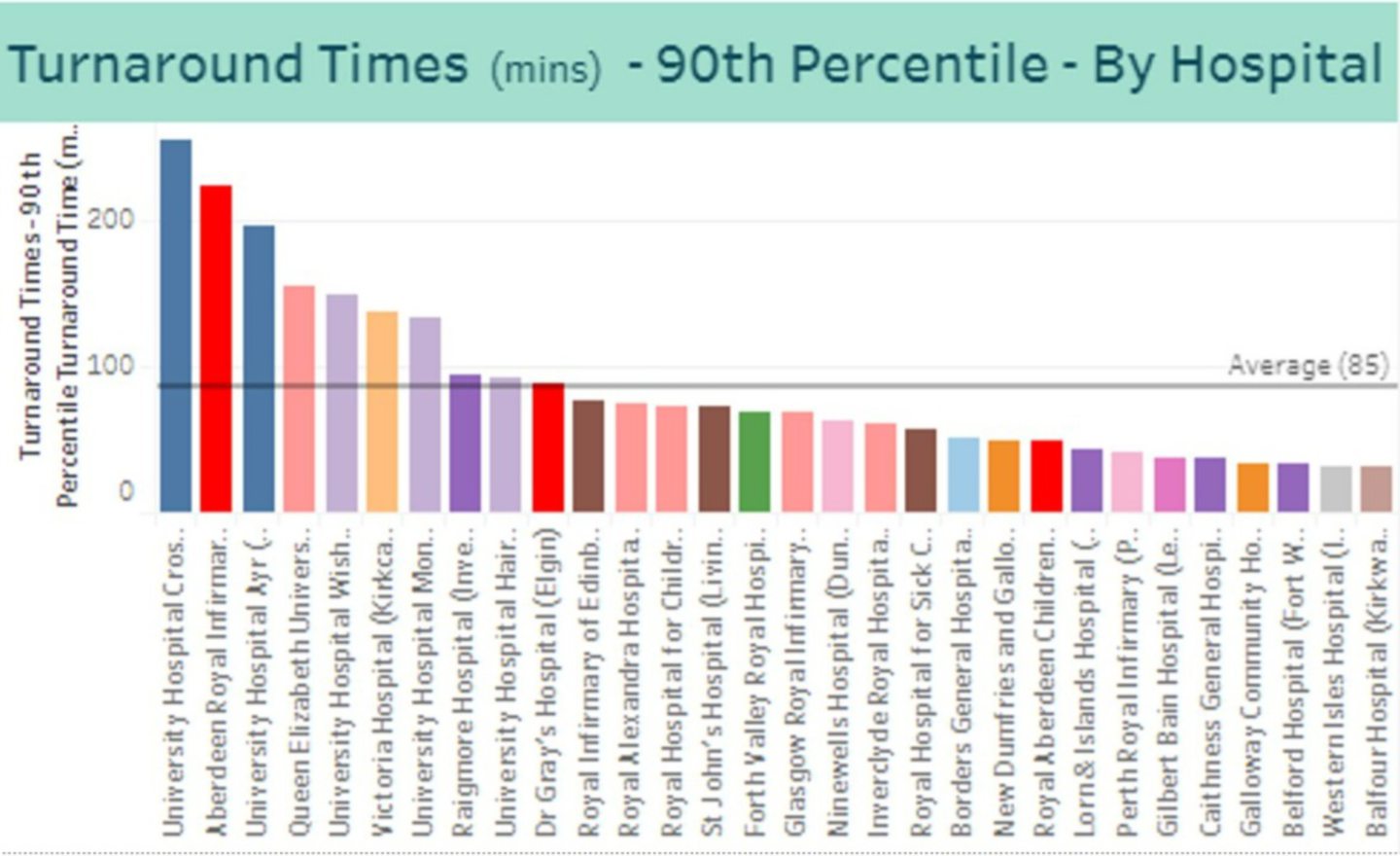
Ambulance turnaround times
Ambulance turnaround times at Aberdeen Royal Infirmary are now at a record high.
Stats show the 90th percentile time is now 223 minutes (3 hours and 43 minutes) – meaning 10% of all waits are longer than this.
This is almost three times the Scottish average of 85 minutes (1 hour 25 minutes), and the second-highest in the country behind University Hospital Crosshouse in Kilmarnock.
Meanwhile, ambulance turnaround times at Dr Gray’s in Elgin have fallen from 90 minutes to 87.
In the week to September 13 there were only two periods, both a few hours long, where no ambulances were waiting outside Aberdeen Royal Infirmary.
Peak times were between 3-8pm, with a high of 15 waiting on September 12 – a level experienced just three other times this year.
A&E performance
Performance has fallen at ARI’s emergency department – and fewer than half of all patients (48.2%) are being seen within four hours.
The hospital recorded its highest-ever number of eight-hour breaches during the week, rising from 94 to 216.
Additionally, there were 52 patients waiting more than 12 hours to be seen at A&E – the second-highest on record for the hospital.
Four-hour performance at Dr Gray’s rose to 76.1%, while it increased to 90.9% at Royal Aberdeen Children’s Hospital.
Ward capacity
NHS Grampian has warned hospitals across the region are almost constantly near-capacity.
In some cases, such as Royal Cornhill, it has exceeded 100% on a number of occasions.
And this is despite a slight increase in the number of beds available – rising to 1,812 across all of Grampian.
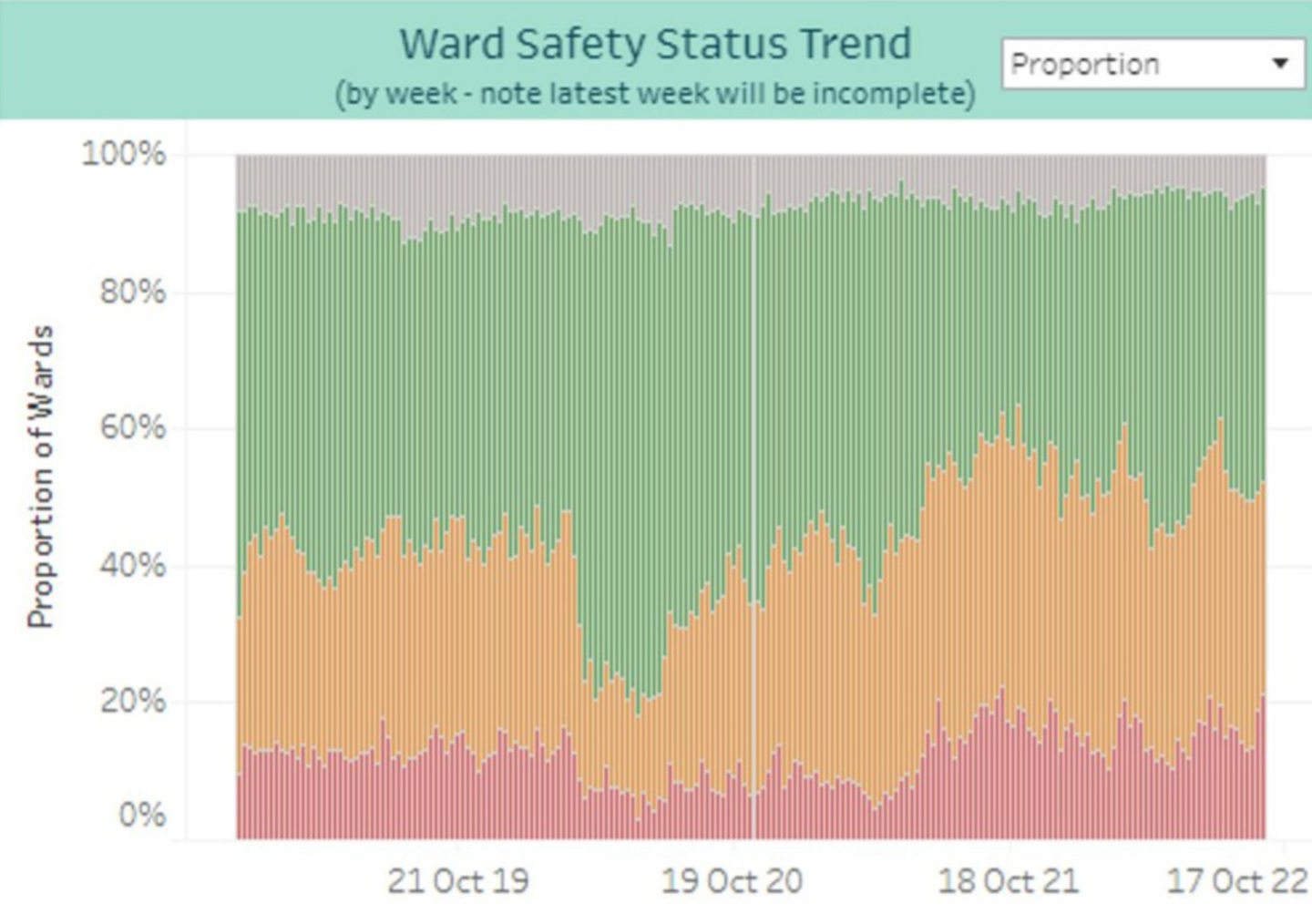
Every day wards they need to rate themselves as green, amber or red in terms of ward safety, with more than half now reporting a red or amber level.
This is often linked to staffing shortages.
Red reports increased to 18.9% the week the stats were compiled – the highest proportion since July.
Financial picture
NHS Grampian finance director Alex Stephen is warning the board that a deficit of £16.9m was recorded at the end of August – “nearly twice the level of our expected plan”.
Across the board, many departments are already in the red.
As a result, it’s updated its forecast for the year from a £20m black hole to £30m.
Mr Stephen wrote: “There is a risk that if as a health and social care system we become used to overspending, that this becomes an accepted cultural norm which is difficult to recover from.”
Already this year NHS Grampian has spent an extra £4.6m on medical staffing, plus £5.2m on locums and almost £3m on nursing.
Soaring inflation is causing problems too, with a 224% increase in gas prices and 23% hike for electricity costing around £5m more.
Additionally, the hospital drugs budget is £1.4m over, partially due to increased activity and vaccination catch-ups.
What’s next?
Unfortunately, the pressures of winter – and potential impact of another Covid surge – are looming over NHS Grampian.
The cost of living crisis and issues with recruitment are only going to compound these further.
Health bosses have committed to three key criteria – maximise staff wellbeing, respond to demand, protect services.
And they say “significant programmes of whole system work” are underway to improve emergency department performance and waiting times.




Conversation