Patients could die as a result of ongoing staffing shortages in Aberdeen, health bosses have warned.
The city’s health and social care partnership says it’s “almost certain” that difficulties with recruitment and retention will have an “extreme” impact on services in the city.
Concerns have also been raised about access to the likes of care homes and dentistry, and the ability to balance the budgets at the end of the year.
The situation has been branded “precarious” by one MSP, calling for action to better look after health staff and encourage a new generation to sign up.
How the ‘post-Covid landscape’ is affecting staffing
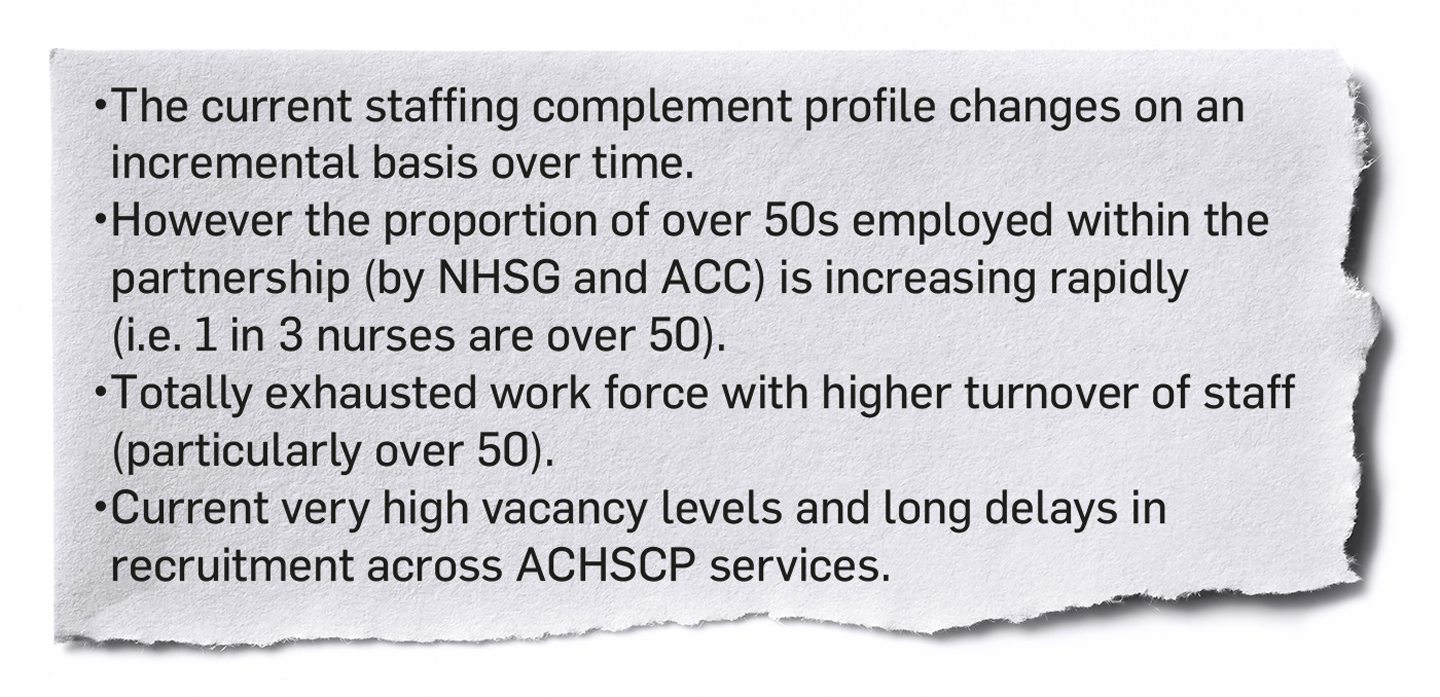
A new report, to go before a city council committee next week, lays bare the full scale of staffing concerns in Aberdeen.
It says one-in-three members of health and social care staff employed by the partnership and NHS Grampian are now over 50.
And in turn, the workforce is “totally exhausted” with a high turnover – again with the over-50s particularly affected – and large numbers of vacancies.
Health chiefs say they’re now in “direct competition” with non-clinical posts elsewhere.
And the cost of living crisis “will impact” on staff members’ ability to get to work because of rising fuel prices.
The report reads: “[We are in a] post Covid-19 landscape, where many staff have reflected on their personal situation, which has led to increased numbers of early retirement applications, requests for reduced hours and staff leaving the service.”
As a result of this risk, it raises the potential for “loss of life and unmet health and social care needs”.
Increased risk of disruption: ‘Mismatch’ of services
Meanwhile the partnership has increased the risk level of patients not being able to access the services they require.
This includes care homes where “significant gaps” in working with operators have led to a “mismatch” between the physical capacity available, and the “suitability and appropriateness” of it.
It also affects dentistry, where concerns over staffing and training are causing practices to start leaving the NHS.
There are just 10 in Aberdeen currently accepting non-private patients – up from seven in August.
This isn’t a localised issue, however. During the last two months, there have been no NHS dentists open to new patients in Moray, for example.
Financial challenge ‘should not be underestimated’
While there’s been no change to the risk level, concerns about the partnership’s financial position are also being raised.
Inflation, the cost of living, staffing costs and energy prices are all playing a role here.
As it stands, it’s currently forecasting to break even by the end of the financial year, but questions are being raised over how much cash it will have available in future.
The report says “tough choices” may be needed when it comes to reducing or stopping services, depending on how much funding is allocated.
“The scale of the challenge [to become] financially sustainable should not be underestimated,” it adds.
‘Pressing need’ for local plan
North-east MSP Douglas Lumsden says there needs to be a “local first, Aberdeen first” plan implemented to ease the situation.
“The current and near-future position of health and social care in Aberdeen looks precarious,” he said.
“Without question, we need to look after these valued professionals more carefully, so they don’t leave the service.
“More needs to be done to make care and nursing more attractive to school leavers and graduates.
“Doing that will avert this pressing risk to our vulnerable and elderly people.”
What happens next?
A number of groups have been set up to help mitigate some of these risks and look for the best ways of working.
Bosses say they’ve “significantly” increased their emphasis on staff wellbeing, embracing new technology and flexible working to help as well.
They also receive regular updates from across the service to help monitor trends and identify problem areas before they spiral out of control.
A more detailed workforce plan is expected to be presented later this month.



Conversation