It’s getting cloyingly hot in the ward as I take my first look at Frank.
A male in his thirties, Frank was assaulted outside a fast-food restaurant on Union Street earlier that evening and rushed to Aberdeen Royal Infirmary.
He appears unresponsive but A&E doctor Craig Brown, who is buzzing around Frank, tells me to attempt contact.
“Hi, Frank,” I say, as sweat pricks my scalp. “Uhmm, how are you today?”
A guttural scream emerges from Frank’s lips.
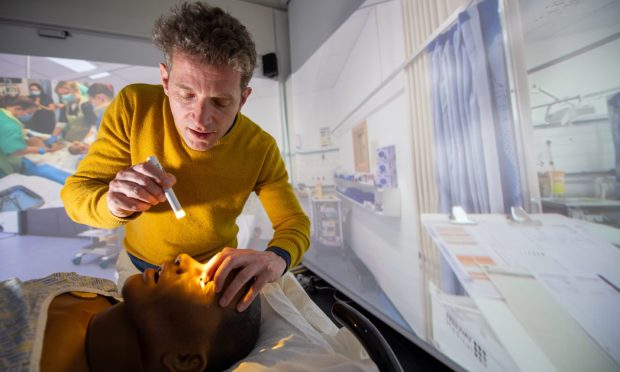
“He’s conscious but not fully normal,” says Craig, handing me a pen light. “Check his eyes.”
Phew, I think. I’ve seen this on TV. Suddenly, the ground feels a bit more solid.
Channeling my inner Charlie from Casualty I shine the light into Frank’s pupils.
Oh, flip! His left pupil contracted. Just like the T-Rex in Jurassic Park!
Realising with dismay that all of my clinical references come from TV and film, I check Frank’s right eye.
Nothing. I try again. Still nothing.
Craig is over my shoulder. “That means a possible bleed on the brain. We may have to operate.”
Oh, Frank, I think. I hope for your sake I’m not doing that as well.
A real-life version of the Star Trek holodeck
Don’t worry. NHS staff shortages have not reached the point where it’s drafting in journalists as doctors.
Not yet, anyway.
Instead, I’m having a go on Aberdeen university medical school’s latest high-tech teaching tool.
It’s called the immersion room, and it is a hands-on, fully-immersive replication of all sorts of situations medical staff may find themselves in.
To me, however, with its video-projector-screen walls that change at the touch of a button, it’s a real-life version of the Star Trek holodeck.
Only instead of beaming down to alien planets to battle rock monsters in a red unitard, I’m a GP resuscitating an elderly woman who’s collapsed in her living room or a paramedic fighting to save a patient in the back of an ambulance.
Or, as you’ve just read, a ward doctor doing a terrible job of diagnosing a man beaten up outside a takeaway.
An important teaching tool for the next generation of doctors
All these scenarios can be played out in the immersion room using the video screen walls and a little bit of imagination. ‘Frank’, meanwhile, is a very expansive dummy with blinking eyes and other moving parts that plays a very convincing patient.
In the year or so since it opened, the room – and Frank – has become an invaluable teaching device for Aberdeen medical school’s approximately 300 students.
“In here, we see the students transition that gap between theory and practice,” says Craig, who along with working on ARI’s frontline is a senior lecturer at the medical school.
“Even though they might be on the wards as a student looking after a sick patient, they are not doing some of the things they’ll have to do when they qualify.”
The room fills in that gap. In doing so, it tries to be as life-like as possible, down to The Jeremy Kyle Show playing on the TV in the elderly patient’s living room TV, or making sure the anesthetist is standing in the right spot in the virtual operating theatre.
Meanwhile, says Craig, it is a safe space where students know they can make mistakes.
The room is entirely controllable, and lecturers can add or remove as many aspects as they want, depending on how much pressure they want to put on the student.
Noise, for example, plays a big role – and not just Jeremy Kyle blaring on the TV.
There’s the noise of a busy operating ward, which can be turned down or ramped up.
Time can also be slowed down – simulator time, that is – to give students more time to think. Or less.
“I’ll tell them,” says Craig, “I’m going to push you to the edge of your comfort zone. But I don’t want to push you too far. I want this to be beneficial for you.”
A test of strength and a journey of discovery
The main benefit I got from the scenarios Craig let me play in was that I probably shouldn’t work in health care.
“Aaaaand there goes his top teeth,” laughs Ian, the lab technician who is controlling Frank through an iPad.
I’m struggling to insert a feeding tube into Frank’s throat using something I can only describe as a medical wrench and Ian is finding it hilarious.
Indeed, Ian’s main reaction to my ineptitude is laughter.
Meanwhile, I’m slowly discovering that a key attribute for a doctor is brute strength. Inserting the tube takes a huge amount of effort – hence why if Frank was a real patient I would have broken his teeth.
Earlier, Craig made me hold an oxygen mask over Frank’s nose and mouth so he could pump air into the dummy’s chest.
With my fingers hooked around the jawbone, it was all I could do to keep the seal tight.
Or not, as Ian pointed out from his corner where he could see Frank still wasn’t breathing.
Entering a strange new world
For my last test, Craig has me perform chest compressions on Frank. Predictably, it doesn’t go well.
“You’ve just broken his sternum,” remarks Ian as I pound out a rhythm to the Nelly the Elephant song, as instructed by Craig.
If I stop just after the “trunk, trunk, trunk” section, then I should have completed the recommended 30 presses.
There’s not much time for a break, though, as I’m back pumping again on Craig’s command.
“A hundred a minute,” shouts Ian, helpfully. I’m sweating by now, and keen to get back to the P&J office where no one puts me in stressful life-or-death situations, virtual or not.
Now, I’m no doctor – clearly – but even I can see Frank’s not going to make it.
The pressure sensors in the dummy show I’m either not pressing hard enough or just not enough in general.
I also lack what Craig calls situational awareness. I’m so focussed on the task at hand that I’m not looking at what’s going on around me, a crucial skill for a hospital doctor and which the simulator aims to develop.
Meanwhile, we’re losing Frank. If he were attached to a heart monitor, I’m sure I’d be listening to that long, continuous beep beloved by hospital TV show directors.
Craig attaches a couple of defib pads (not active, fortunately, or I’d no doubt zap myself) and tells me to stand back.
I stop the compressions and throw my hands in the air. For a moment, I’m a real doctor hoping against hope that my patient will make it.
But then Ian – of course it’s Ian – delivers the bad news. I stopped the chest compressions for too long, and the defib didn’t work.
I feel like draping a sheet over the patient and marking the time of death.
Sorry, Frank.







Conversation