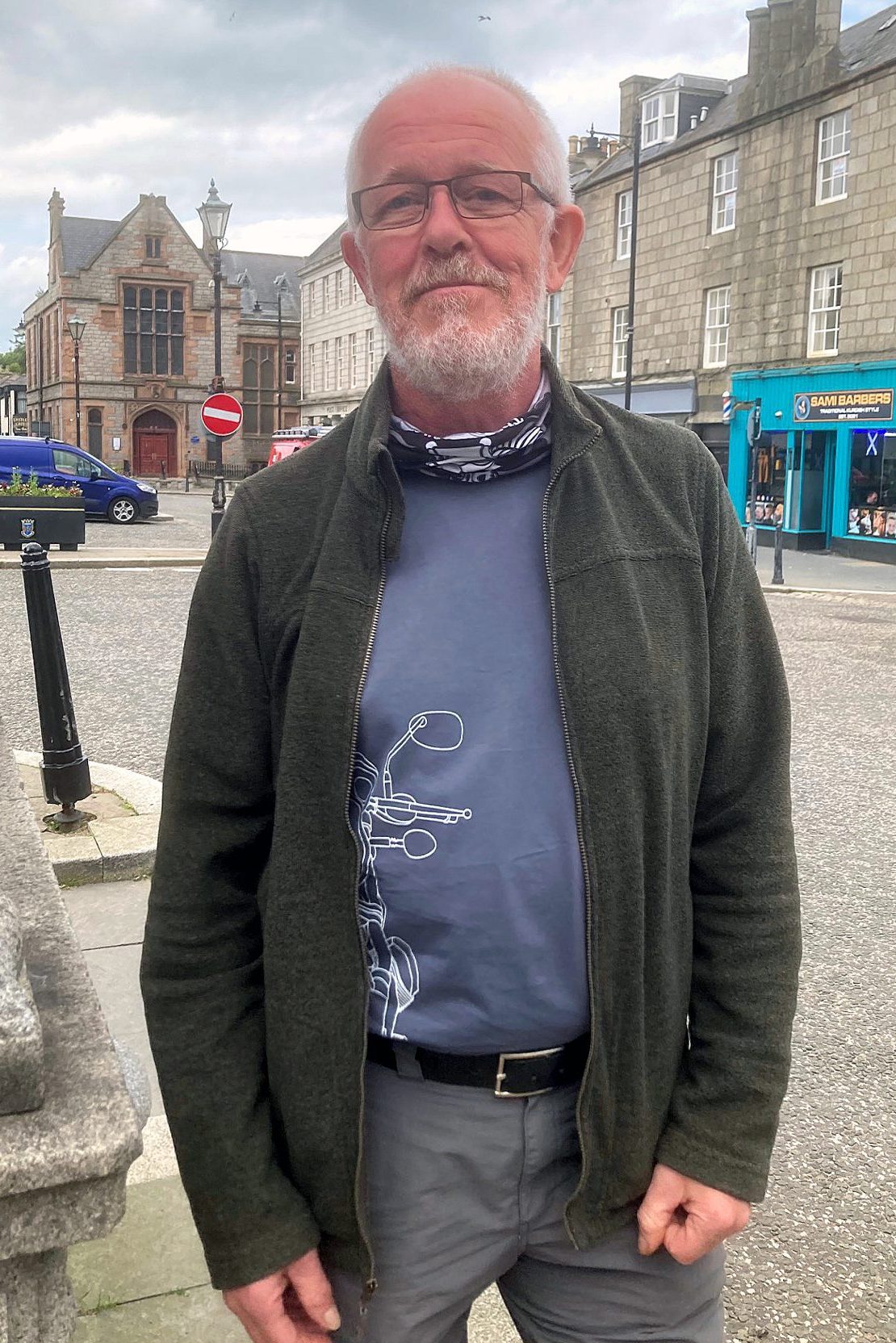
With regret in his voice, David Easton lists the healthcare services available at Huntly’s Jubilee Hospital in 1988.
Back then, the hospital had 55 beds, a 24-hour casualty department, a maternity unit, and long-stay geriatric and psychogeriatric wards. It also had an ample supply of acute beds, the ones reserved for the most seriously ill patients.
David, a former medical director at Jubilee, stops and sighs.
Four decades later, the hospital has just 18 beds, he says, less than a third of the 1988 total.
The specialist wards have disappeared, transferred to bigger hospitals such as Aberdeen Royal Infirmary.
And five years ago the casualty department was downgraded to a minor injuries unit.
David, a softly-spoken Huntly resident who was also the town’s GP for 28 years, falters in disbelief.
“It’s all gone,” he says.
Huntly Minor Injuries Unit and the £20m hole in Aberdeenshire’s healthcare budget
Today (Monday, July 1), Jubilee lost another link in its healthcare when the minor injuries unit (MIU) halted its 24-hour operations and became a day-only service, running from 7am to 7pm.
The Aberdeenshire Integration Joint Board (IJB), which oversees the region’s health and social care services, says the change will save more than £716,000 in the coming financial year as bosses look to plug a £20m budget gap.
Fighting the IJB is David, who along with a determined group of fellow Huntly residents have serious concerns over the changes.
First, they believe the cancellation of a nighttime service at the MIU will heap more pressure on overstretched A&E departments while putting residents in danger.
They also warn that instead of saving money, the change will end up costing NHS Grampian more in the long term.
And finally, they say the decision is the latest example of health bosses chipping away at regional services like the MIU, depriving rural communities of critical care as they prioritise bigger hospitals that are often hours away by car or ambulance.
It reminds David of the time, back in his working days, when he heard an NHS bigwig refer to Huntly and its surrounding areas as just “mountains and sheep”.
“But we’re not just mountains and sheep,” David says. “There’s a lot of people who live in the area and to centralise everything is going to leave a black hole.”
Coffee and criticism as Huntly fights back
On a recent midweek afternoon, David gathers with seven Huntly residents in the back of a Huntly restaurant.
As they sip coffee they share the latest news of their grassroots campaign to fight the MIU’s nighttime closure, launched when the decision was made public in March.
Like the coffee, the mood is black. They have yet to hear the IJB’s confirmation of the closure, which comes several days later on Friday June 28. But they know the odds are against them.
Two days previously, at a community hearing, the campaigners had a 3,002-name strong petition rebuffed (though it was grudgingly accepted later).
An online petition with more than 8,000 names (and counting) is being similarly ignored.
The nighttime closure, admits David, is “probably a done deal.”
But, he adds quickly: “We must keep shouting.”
The stakes are already too high.
Why ‘minor injuries’ is misleading
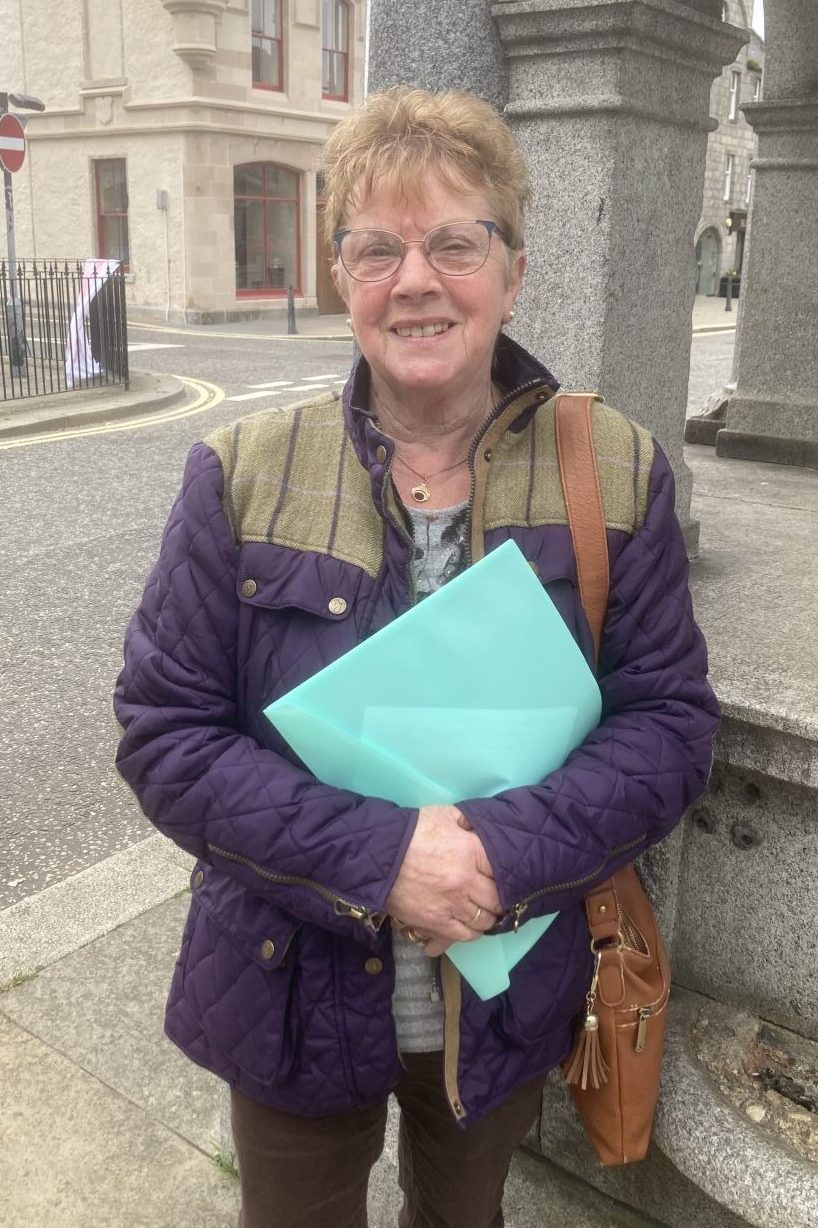
“This is the frightening bit,” says Anne Christie. “Lives are going to be lost.”
As a former minor injuries nurse, Anne knows first-hand how important the unit in Huntly is.
Don’t let the name mislead you, she warns. ‘Minor’ simply means non-life-threatening. Staff at the MIU regularly treat broken bones, eye injuries and “lots of lacerations”.
Local farmer Paul Smith still has all ten of his fingers because of the Huntly MIU. Staff successfully sewed a severed digit back on after his hand got trapped under a falling log pile.
“It’s not something that you can just put sticking plaster on,” Paul says.
Meanwhile, closing the minor injuries unit from 7pm to 7am will have knock-on effects, say residents, funneling more patients to A&E departments already struggling under weight of numbers.
“So the system just becomes totally overloaded,” David explains, pointing to recent news stories of ambulances stacked outside ARI. “As it already is, but more so.”
The argument that the closure will save money is similarly short-sighted, he says.
David calls it the “slopey shoulders” effect — patients who would have been seen at the MIU will have to go elsewhere. So the £716,000 saving touted by the IJB simply lands on another health care service, or even the ambulance service or police.
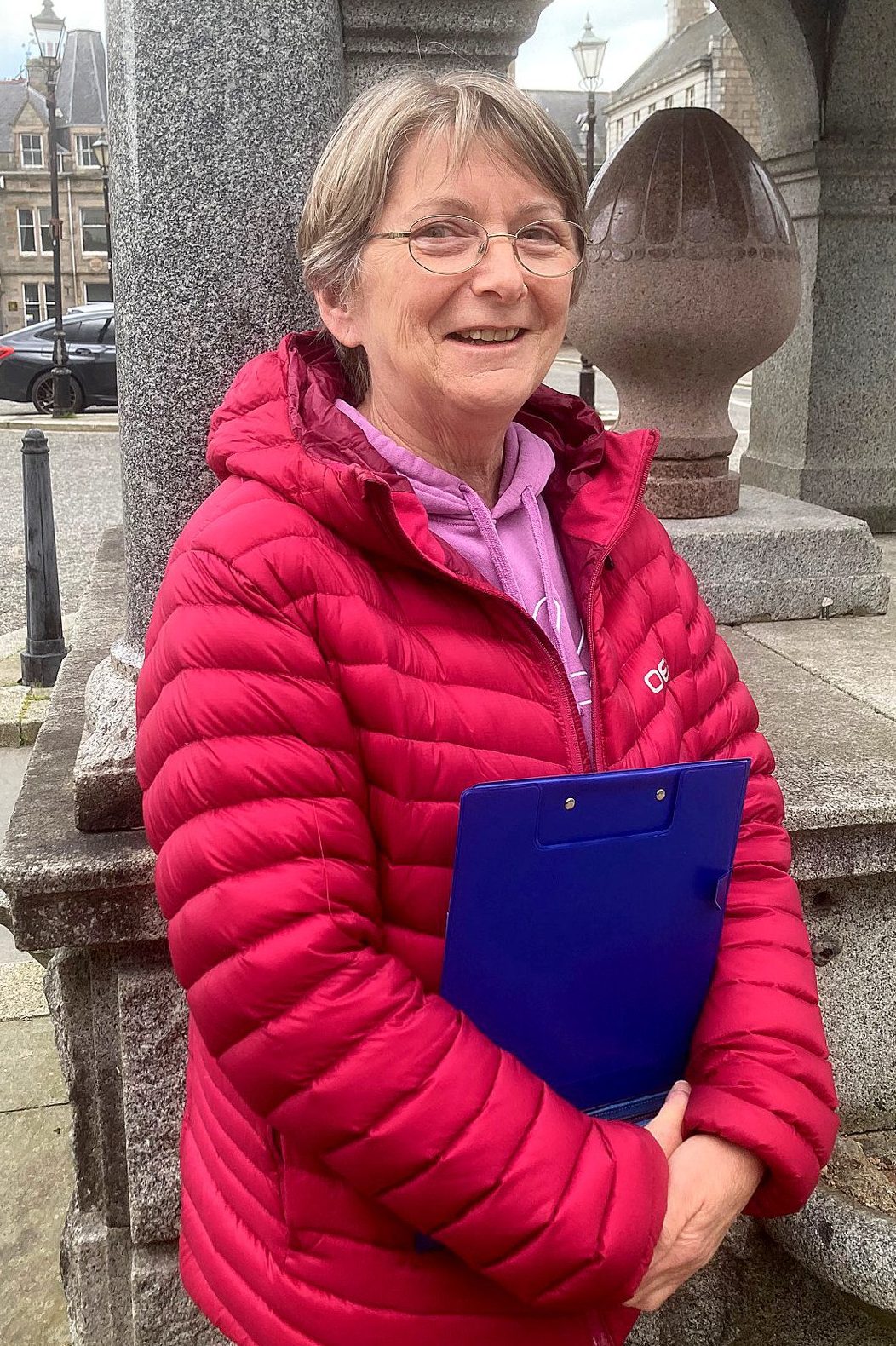
“They needed a quick fix,” says Sheena Watchman, a retired NHS health records manager who sits through the meeting with a large stack of papers on her lap.
“It was, ‘how are we going to save this money?’ And they’ve just barged ahead.”
The beginning of the end for rural healthcare
As well as their anger over the hollowing out of Huntly’s healthcare, the residents talk of something else — a feeling the IJB won’t stop chipping away at Aberdeenshire services.
“They’re sharpening the pencil so much, but at the end it’s going to break,” chides Dorothy Anderson, a former nurse at Roxburghe House, the palliative care unit in Aberdeen.
The consensus is that the nighttime service cut is the first step in closing down the MIU altogether, or even Jubilee Hospital.
“I can see the pattern,” someone says. “And the decision has been made.”
The residents even suspect the IJB of finessing the numbers to support its decision to cancel Huntly MIU’s nighttime services.
In March, the IJB declared that the unit sees a daily average of just four patients between 6pm and 8am, a number that IJB chair Anne Sinclair called “very low”. In the four months to the end of February, only 69 patients attended during those hours — and on 17 nights no one showed up at all.
But the residents claim that at least two late-night patients in Huntly who should have been seen at the MIU were directed by call centre handlers to Aberdeen Royal Infirmary.
“It was intentional,” says Anne Christie, the former minor injuries nurse and one of the two patients.
In response, the Aberdeenshire Health and Social Care Partnership, which is overseen by the IJB, said the allegation call centres are sending patients to ARI to keep the numbers low is “categorically not true” and that the unit sees an “exceptionally low number of people with minor injuries”.
It also said it anticipates “no impact” on ARI’s emergency department from the changes because the MIU treats injuries that do not require emergency care.
“The very nature of a minor injury is that it can wait to be seen,” an AHSCP spokesperson said.
The spokesperson added there is “no plan” to close Huntly’s MIU.
‘One of the worst-performing health boards of all’: Services cut across Aberdeenshire
If you are looking for evidence of diminished regional services, you don’t need the to look far from Huntly.
Insch, 20 minutes down the A96, lost its hospital five years ago despite a concerted rescue campaign by locals. The minor injury units in Buckie and Keith closed during Covid and never reopened.
Meanwhile, the minor injuries units in Fraserburgh and Peterhead also had their nighttime services cut.
As of July 1, across the whole of NHS Grampian, only Dr Gray’s Hospital in Elgin and ARI in Aberdeen will be able to take nighttime patients.
“Someone will die,” warns Dawn Fraser, who until she retired last year worked in the Peterhead MIU and now campaigns on its behalf.
“I can’t begin to tell you the amount of people whose lives have been saved in these units.”
Back in Huntly, David says NHS Grampian has become a “privatised service by default”, especially in rural areas where more than a quarter of the population are over 65.
Shorn of public options, patients are either paying private providers — if they can afford to — or playing a healthcare lottery where the odds look increasingly grim.
In April, Public Health Scotland revealed NHS Grampian cancer patients suffer the second-longest wait times for treatment, behind only Shetland.
“Grampian is one of the worst-performing health boards of all in terms of all the things you want it to be good at,” David seethes. “Your cancer care, the time it takes to get seen, your first consultation with a consultant et cetera. We fail in all of those.”
‘The NHS as we know it has crumbled’: Does Huntly Minor Injuries Unit have a future?
The coffee is finished but the mood remains black.
A retired nurse who worked in England tells the room about the smaller district hospitals south of the border that were absorbed into so-called “mega-trusts”. The fear is that the same will happen in Scotland.
“The NHS as we know it has crumbled,” someone says, glumly. “Past tense.”
A week and a half later, on a phone call from Huntly, David’s mood is even darker.
He’s read the P&J news story on the IJB’s confirmation and is angry that none of the residents’ concerns have been addressed.
There is talk of legal action. Sheena, with her stack of papers and inside knowledge of how NHS public consultations are supposed to be held, is adamant correct procedure has not been followed.
Meanwhile, the residents are incensed their campaign has been ignored — the 3,002 names on the petition, plus the online signatories (now up to 8,200).
But mixed with the anger is sadness. Yet another piece of Huntly’s healthcare has been quietly dismantled.
“It is a very large chunk of the service being taken away,” David says, before remembering what has already been lost.
“One of many over the past 20 years.”




Conversation