
Leanne Watson’s mum Kate was nearly two years into her retirement in January this year when she started to experience pain in her leg.
The former special needs teacher at Albyn School brushed it off at first and still managed a weekend mother-daughter shop and coffee.
However, when it got to the point Kate could not sleep on the evening of Sunday January 28, they decided to call 111.
By 11am on Tuesday morning, after being diagnosed with sepsis, Kate was dead.
Speaking about it eight months on, Leanne said even now she still has nightmares about those two days which involved her and her dad, Allan, dragging her mum into the car to the hospital after ambulance delays.
Recalling those devastating 48 hours, Leanne said: “It’s a real panic because you don’t know what it is, and you can see her practically dying in front of your eyes, and you don’t know what to do.
“It’s really traumatic.
“In a matter of three days, you can go from being perfectly healthy to dying of sepsis.”
In this article, Leanne recounts the painful experience and what followed afterwards including:
- Leanne and her dad dragging her mum into the car to the hospital after being told they could be waiting six hours for an ambulance
- What it was like appearing at ARI and struggling to find anyone to help
- The health services involved including Aberdeen City Health and Social Care Partnership, Scottish Ambulance Service and NHS Grampian apologising and commenting on Kate’s treatment
- How Leanne is helping raise awareness for sepsis in her mum’s memory in Aberdeen, and the key signs everyone should look out for
Kate was getting worse by the second
Even now, her family do not know how Kate, 70, got the infection (necrotising fasciitis) that caused the mum-of-two to have sepsis.
Sepsis cannot be caught virally but arises from the body’s response to an infection with the immune system going into overdrive.
After Kate suffered a sleepless night filled with extreme pain, on Monday January 29 at 11.30am Kate’s husband called 111 and their daughter Leanne, who thankfully was visiting from London at the time, came round to help.
Three hours later at 2.30pm, two advanced nurse practitioners (ANPs) arrived at their home in Balmedie.
At this point, Kate had deteriorated.
“My mum seemed confused,” said Leanne. “She was getting worse by the second but I didn’t know what it was.
“When the ANPs took the cover away to look at her leg, there was a massive black patch.
“But it hadn’t been there an hour earlier. Me and my dad were like, this is serious… she’s not eating or drinking.
“They took all her vitals but seemed to say they think it’s a blot clot.”
The nurses went to the living room to call the Acute Medical Initial Assessment Unit (AMIA) at Aberdeen Royal Infirmary and the Scottish Ambulance Service (SAS).
When they came back through they said they had asked for an ambulance to be there within the hour.
But they said to call 999 if Kate got any worse.
The ANPs then left the house.
Ambulance delay warning of SIX hours led to ‘dramatic’ action
Leanne said: “About two hours later no ambulance arrived and she was really confused and slowing her speech.
“We called 999 and said we need an ambulance now because it’s got much worse.
“And they said ‘It’s going to be six hours’.
Leanne made a choked sound of disbelief: “Six hours.”
But the shock wouldn’t stop there, as the 999 call handler proceeded, according to Leanne, to inform her that A&E was “closed”.
Leanne continued: “We said, ‘We can’t wait six hours, she’s getting worse by the minute’.
“They said, ‘There’s nothing we can do about it A&E at ARI is closed.
“We said ‘Closed?’”
“‘Yes, there’s this massive queue of ambulances outside and it’s closed. They’re not taking anybody.'”
By around 4.30pm on the Monday, Leanne and Allan made the decision to take Kate in themselves but by this point, she could not walk.
“So as dramatic as it sounds we had to drag her through the house out of bed,” said Leanne.
“We had to drag her into the car which was a nightmare because she’s in pain and because she was like a dead weight.”
She just kept saying ‘I feel like I’m dying’ at Aberdeen Royal Infirmary
They eventually managed to get her into the car and arrived at Aberdeen Royal Infirmary near the main entrance.
But upon parking up at 5.15pm they struggled to get hold of anyone. Leanne’s dad ran into the reception near where they parked and desperately tried the phones while Leanne ran to grab a nearby wheelchair.
In her confusion, Kate tried to get out of the car and slammed into the pavement.
“I couldn’t get her up,” added Leanne. “And this is January, it’s freezing and she’s lying on the pavement.
“There was absolutely nobody around.
“I was shouting for anybody to come and help. And luckily, this doctor who had just finished his shift and was leaving came over to help.”
The doctor tried to call different departments but could not get hold of anyone. By this time, a few others came over to help including a porter who offered to take them to Ward 101.
When they arrived, they were asked to wait but Leanne knew they could not waste another minute.
“She just kept saying ‘I feel like I’m dying’.
“By this point, my mum was completely unaware, she looked awful, couldn’t move and she was in absolute agony so we insisted that they get a doctor.
“So they did and then once she was in, they were really good.
“The minute the surgeon lifted up the sheet he said it was sepsis in two seconds.”
Kate was rushed into surgery to remove the entire patch on her thigh. While she survived and was put into an intensive care unit, by Tuesday morning the sepsis had caused her organs to start failing.
She suffered a heart attack at 11am and died.
Questions about ambulance delays and early treatment
The loss of her mum and the “traumatic” build-up to getting her into hospital have left Leanne with a lot of personal guilt and questions on whether more could have been done to save her mum and catch the sepsis earlier.
She said: “The problem with sepsis is every hour counts so it leaves you feeling really guilty because you wonder, if you had taken her in earlier, would she have survived?
“I didn’t know about sepsis. I didn’t know what to look for.
Speaking in particular about her mum’s treatment, Leanne added: “Once she was in ARI her treatment was really good. It’s just the build-up to it and getting there.
“And the doctor seemed to immediately know it was sepsis which I wish they [The ANPs] had before because the patch of skin was exactly the same at that point.
“And maybe it wouldn’t have made any difference but, you don’t know.
“We were told that if we hadn’t taken her to hospital, she would have died in agony at home that night, which would be awful.
“I know the health services are busy but half an hour is probably the maximum you should wait when you’re telling the operator it’s extremely serious.
“I shouldn’t have to drag my mum to hospital.
“My mum’s last moments were lying outside in winter and she couldn’t get up.
“It’s not the individual doctor and nurse’s fault, it’s the system as a whole that is failing.”
Granite City Sepsis set up in Kate’s memory, and the signs to watch out for
Since losing her mum, Leanne started to research sepsis and wanted to do something to help raise awareness.
Only coming across one main charity, The UK Sepsis Trust, Leanne decided to set up a local Facebook group.
Called Granite City Sepsis, Leanne has distributed leaflets and posters to make sepsis symptoms more recognisable and has spoken about her mum’s story to help raise money for charity.
Her hope is to one day raise enough funds to set up a support group for sepsis sufferers who are often left with disabilities and medical conditions and their loved ones.
She also wants to help fund more sepsis training and campaigns within the health services in the north-east.
“If there was a bogeyman of the medicine world it’s sepsis because it’s hiding in the dark and nobody’s talking about it,” said Leanne.
“It kills really quickly. Sepsis is a bigger killer than breast, bowel and prostrate cancer put together. It kills 48,000 people a year and worldwide it kills more people than cancer but you just don’t hear about it.
“Unfortunately, people’s stories about them dying or losing limbs is the only reason we’re hearing a bit more about it, which seems too late.
“It’s difficult to criticise the NHS because they do mostly a great job but since starting Granite City Sepsis, I’ve been inundated with stories from people who were let down.”
‘My mum was let down when she really needed it most’
When her mum died, Leanne said the family were inundated with letters from former pupils and parents talking about the impact her mum had over her 20 years at Albyn School.
For civil servant Leanne, who would always hear from her mum about “her kids” on one of their numerous daily calls, she said: “You don’t really realise at the time how much impact she’s having.
“One parent wrote that my mum’s kind and encouraging words and great patience shown to her boys would be carried with them throughout their lives.
“We’ve had lots of kind of comments like that because a lot of the children that came were really struggling but a lot went on to be really successful. She’s got loads of success stories.”
Leanne added: “It’s definitely my mum that drives me and I feel she was let down when she really needed it most.
“She was someone who seemed to have made such an impact with what she did… she impacted my life so much. She was planning on helping kids here and there in her retirement.
“This is something everybody’s lost out on.
“And it’s sad to think that her final hours were so traumatic.
“My mum just deserved better.”
Kate’s family raise concerns
Following the incident, Leanne and her dad put in a complaint with NHS Grampian and also had former MP Richard Thomson email on their behalf.
Leanne raised her concerns about her mum’s early treatment regarding the identification of sepsis, staff training around the condition, the ambulance response time and advice given by the SAS and their difficulty in reaching anyone when they arrived at ARI.
They eventually got a detailed response five months later addressing their concerns.
Kate’s treatment was split between four health organisations: NHS 24, Scottish Ambulance Service (SAS), the City Visit Service run by Aberdeen City Health and Social Care Partnership (ACHSCP) and NHS Grampian.
Health services apologise for ‘care in some areas falling short’
Addressing the complaints mentioning the visit from the advanced nurse practitioners (ANPs) at Kate’s home, chief officer for the ACHSCP, Fiona Mitchelhill, said: “I am deeply sorry that Mrs Watson’s care in some areas fell short of what should be expected.
“I would offer my deepest condolences to her family and assure them that we have carried out a thorough investigation into all the circumstances to ensure that we make the necessary improvements.
“I also apologise for the delay in responding to the family. This was a complex matter, involving several services which dealt with the different stages of her care. We have reviewed our procedures to ensure that such a delay does not happen again.
“With regard to sepsis management, I would like to stress that the City Visiting Team are dedicated to providing the most professional care.
“All staff are trained in advanced life support and use a well-proven sepsis-screening app for calculating a National Early Warning Score. This is automatically done at every visit, regardless of symptoms.”
She said this score is then discussed with “acute medical initial assessment professionals” and a plan is put in place to manage the patient’s condition.
With regards to training, Ms Mitchelhill said all staff also receive additional sepsis course training.
SAS mentions high demand and long handover times
A spokeswoman for the SAS extended the service’s “sincere condolences” to Kate’s family for their loss and said: “We can confirm we received a call from the City Visiting Service at 3.28pm to request a non-urgent ambulance transfer.
“The caller was advised that an ambulance response could be delayed due to extremely high demand on the system that day.
“We received a further 999 call at 4.46pm and this was triaged for a clinician call back to further assess Mrs Watson’s condition.”
The spokeswoman said an advisor kept in contact with the family until they arrived at the hospital. This was disputed by Leanne and Allan.
In addition to the high demand on services, they mentioned the average handover time for ambulances at ARI at the time was one hour and 51 minutes which they said would delay their crews from getting back on the road to treat other patients.
The spokeswoman added: “We continue to work with NHS Grampian in addressing these hospital delays but acknowledge the limited progress.
“An investigation into Mrs Watson’s care was carried out and recommendations relating to our part of her NHS care journey were implemented in full.”
NHS Grampian address ambulance turnaround times and thank family for praise of hospital staff
A spokesman for NHS Grampian said: “We would like to express our sincerest sympathies to Mrs Watson’s family for their loss.
“NHS Grampian’s Acute Medical Initial Assessment (AMIA) unit stated to the City Visiting Team that Mrs Watson should be admitted to hospital for further examination, prior to SAS being called at 3.28pm to provide transport.
“When patients arrive at our hospitals they are seen based on clinical priority. Those in need of emergency care, as in Mrs Watson’s case, are seen with the utmost urgency.
“Average ambulance turnaround times are not indicative of the time taken for emergency cases to be seen.
“After arriving at AMIA Mrs Watson was promptly examined, diagnosed and taken for surgery.
“It was incredibly kind of the family, at what was undoubtedly an incredibly difficult time for them, to praise the professionalism of our AMIA and intensive care unit teams.
“We’d assure the family that this has been fed back to the staff who cared for Mrs Watson, in hospital, and was very much appreciated.”
In response to the family’s personal complaint about their visit to ARI, Fiona Mitchelhill from the ACHSCP apologised and said: “While it may be of little comfort to the family, had they presented to the Emergency Department entrance, staff would have been available to support them as the department is open 24 hours a day, every day.
“I am sorry that you were informed this was closed as I can assure you this was not the case.”
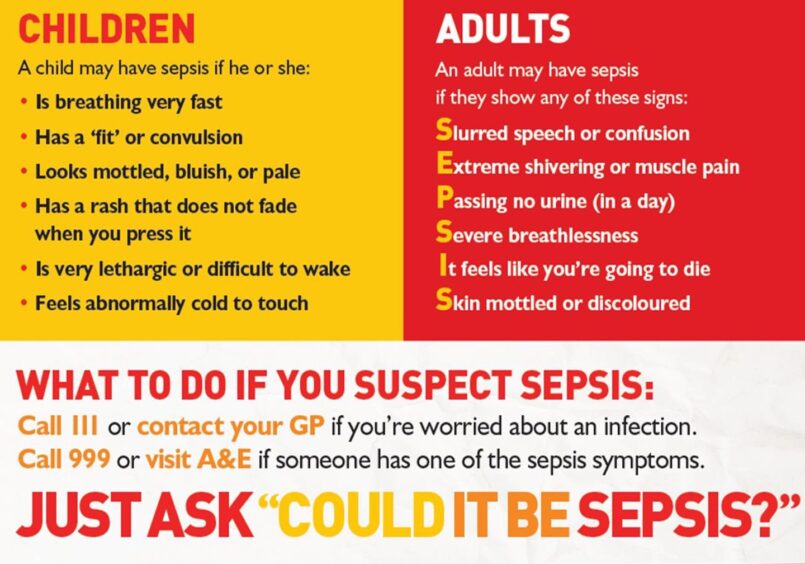
Sepsis symptoms
The symptoms of sepsis can be difficult to spot. For how to check for the condition in adults, UK Sepsis Trust said to check for:
- Slurred speech or confusion
- Extreme shivering or muscle pain
- Passing no urine (in a day)
- Severe breathlessness
- It feels like you’re going to die
- Skin mottled or discoloured
If you or another adult develops any of these signs, it is important to seek urgent medical attention.
For more information on sepsis visit the NHS website. For additional information or to get in contact with Granite City Sepsis, visit the Facebook page.











Conversation