The Scottish Government has been urged to take urgent action to address bed-blocking after it emerged the problem cost health boards in the north and north-east £23 million last year.
Statistics obtained by the Scottish Conservatives have laid bare the financial impact of patients being kept in hospital despite being healthy enough to leave.
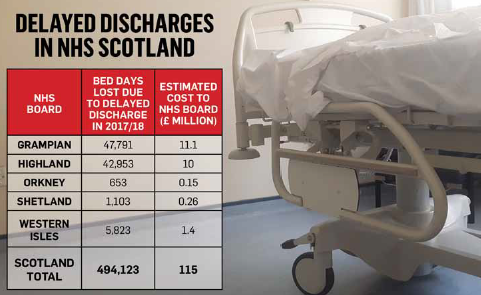
Delayed discharge cost NHS Grampian £11 million and NHS Highland £10 million in 2017, Orkney £150,000, Shetland £260,000 and the Western Isles £1.4million.
The human cost was of that was delayed treatments and patients – in particular the elderly and those with chronic illnesses and disabilities – unable to return home.
An NHS spokeswoman last night stressed that action plans were being drawn up to ensure patients could be more speedily transferred into community care, but warned there would be “no quick fix”.
Tory MSP for Aberdeenshire West, Alexander Burnett, said the figures should be a “source of shame” for health secretary Shona Robison, who vowed to “eradicate” delayed discharge three years ago.
“For the north of Scotland, this £23 million could be far better spent on treating patients who require medical attention,” he said.
Councillor Jenny Laing, co-leader of Aberdeen City Council and member of the Integration Joint Board (IJB), is urging the Scottish Government to increase funding to let the local authority address the issue.
She said: “Delayed discharge figures have improved in Aberdeen thanks to the IJB’s delayed discharge action plan, which was implemented in 2015.
“Delayed discharge disproportionately impacts upon older adults and adults with chronic illness and long-term disabilities.
“I would urge the Scottish Government to stop cutting back on council funding in order to allow the council to increase investment in social care provision to help solve the bed blocking problem.”
The Scottish Government argues that “good progress” is being made in reducing bed-blocking and has highlighted the massive investment in social care being made.
A spokesman said: “In Aberdeen City, where there is good progress with integrating health and social care services, we are seeing reductions in the number of bed days lost to unplanned admissions, including bed days lost to delayed discharge.
“We expect boards to keep working hard to ensure no patient has to spend unnecessary, extra time in hospital and have transferred around half a billion pounds from the NHS into social care and integration this year, while the health budget will increase by almost £2 billion by the end of this parliament.”
The majority of patients whose discharge from hospital is prolonged find themselves lingering in hospital because of delays in the social care system.
A spokeswoman for NHS Grampian insisted that “action plans” were being drawn up to resolve the issue.
She said: “Delayed discharge is frustrating for the patient, their relatives and our clinical teams.
“The IJBs aim to provide a seamless response to the health and social care needs of people in Grampian.
“All areas have action plans which deal with short, medium and long term approaches to delayed discharge.
“It must be stressed there is no ‘quick fix’ for this issue.”
Last June, the Aberdeen Integration Joint Board devoted £47,000 towards converting two properties into accommodation for people leaving hospital.
The move followed a scheme pioneered by Moray’s IJB, which opened a £120,000 “halfway house” between hospital and home in Elgin last March.