The key symptoms of NHS Grampian’s current crisis have been revealed as north-east patients continue to bear the brunt of a system in turmoil.
Poorly residents have been left lingering on waiting lists for months, and even years in some cases, while those needing emergency treatment can be left in ambulances outside the hospital for hours.
At the weekend, the P&J revealed the tragic plight of former teacher Kate Watson – who died of sepsis after her family had to “drag” her to Aberdeen Royal Infirmary (ARI).
Meanwhile, a Torphins mum was forced to give a newborn baby CPR during a terrifying wait for an ambulance.
Months earlier, it emerged that there were no ambulances available to send to Balmedie when a toddler died in a car park – due to five-hour waiting times.
And an increasing number of women recovering from cancer surgery are pleading for action as they wait years for reconstruction procedures.
North-east health bosses admit the performance is “not what anyone wants to provide”.
And in a recent annual update, NHS chiefs laid bare the main causes for the north-east crisis.
Here we outline the seven key factors.
Is money at the root of NHS crisis in the north-east?
It was against a chaotic backdrop that Alison Evison, the chairwoman of the NHS Grampian board, addressed attendees at the summit in Elgin.
She explained it had been a “challenging year for the NHS across the UK”, and presented an overview of the biggest issues.
Money is at the heart of the matter.
Mrs Evison said that NHS Grampian has a total budget of £1.53 billion, but 40% of this is delegated to Aberdeen, Aberdeenshire and Moray health and social care boards.
And the budget has to cover the wages of about 17,000 people, with the body the “largest single employer in the north-east”.
Facing inflation and soaring costs for everything from medicine to power, the health service is spending £78 million more than it should at the moment.
There is, Mrs Evison added, a “serious need” to look at savings.
“This is a very serious issues for us, and underlines everything we are doing as a board.”
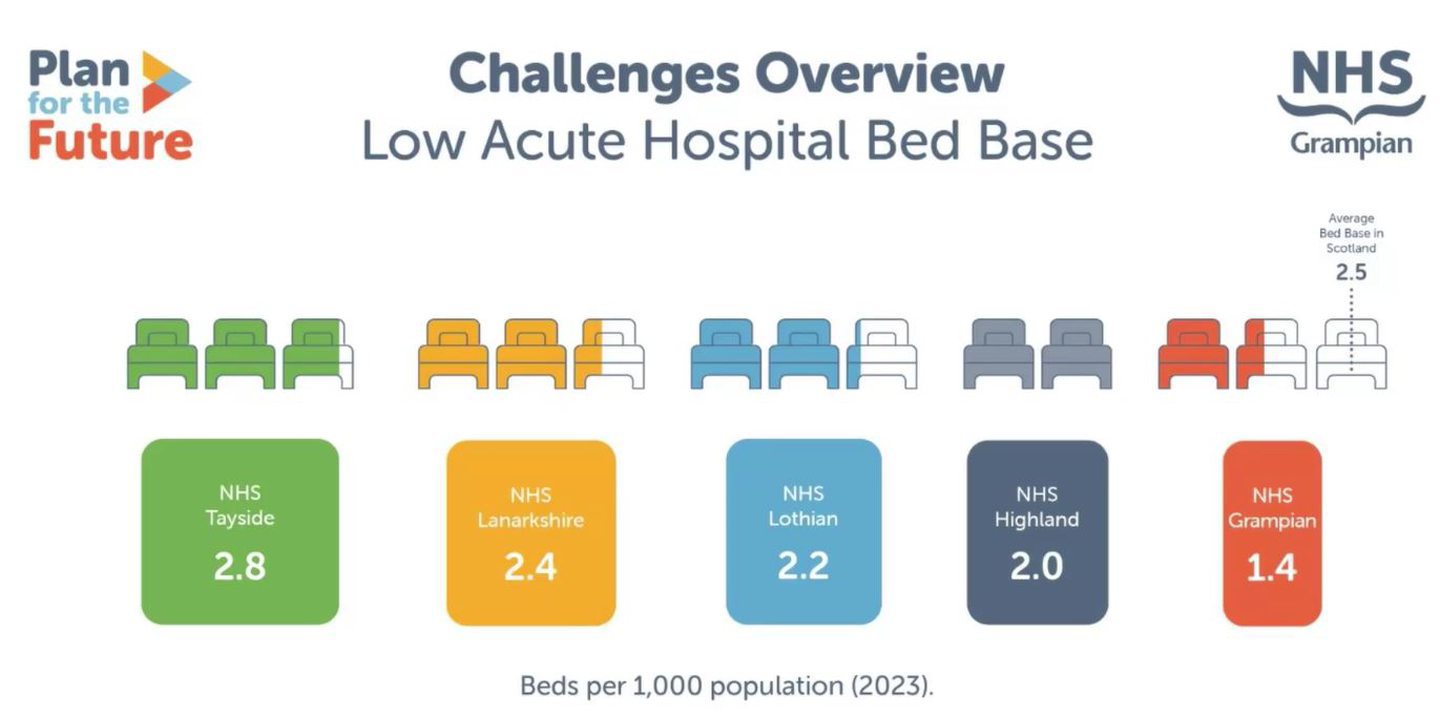
NHS Grampian’s lack of beds compared to other parts of Scotland
Mrs Evison said another huge hurdle is NHS Grampian’s lack of beds compared to other parts of Scotland.
She beamed figures onto a screen showing how the area fares in comparison to others – with NHS Tayside having double the number.
“No other board has fewer than two beds for every 2,000 people,” Mrs Evison told the room.
This is “at the heart” of the waiting times patients can be forced to endure when turning up at Aberdeen’s beleaguered emergency department.
Could things get any better?
A recent review indicated that the north-east board needed another 12o beds in its “acute settings”, which refers to A&E and surgery departments.
“The only way to substantially improve performance is to open more beds,” the chairwoman admitted.
However, while the planning process to secure more has got under way, Mrs Evison warned people not to get their hopes up.
“Lack of funding means it is extremely unlikely we will be able to undertake this reform to introduce further capacity at present.
“We are endeavouring every day to maximise bed space in our hospitals, and to run our system efficiently.”
Ageing buildings need work
NHS Grampian’s most problematic buildings include Dr Grays Hospital in Elgin, where theatres, the mortuary, maternity wards and the emergency department all require work.
At ARI, surgical wards, operating theatres and the laundry are in need of upgrades.
Recently, the decontamination unit at Foresterhill in Aberdeen has suffered four “failures”.
This meant that 100 operations had to be cancelled.
However, there’s no money to replace it right now so bosses will keep it running.
When they can afford to fix the ailing unit, in the years ahead, there will be a “planned shutdown”.
Massive size of NHS Grampian area worsens crisis for north-east patients
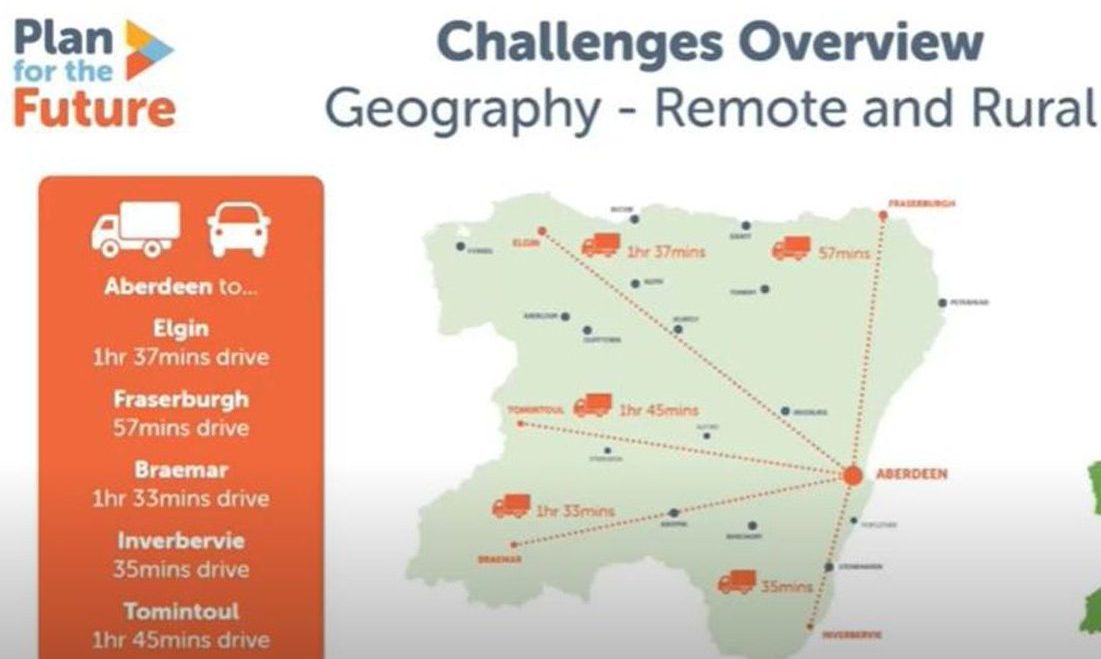
The crisis-hit north-east NHS board covers a staggering 33,500sq miles.
That puts it roughly on a par with countries like Puerto Rico and Cyprus.
Mrs Evison explained: “Whilst an extremely beautiful part of the world, it brings its challenges.”
This means that NHS services are carried out from more than 100 locations, and patients in Braemar are about 90 minutes away from the flagship hospital in Aberdeen.
And one particular challenge leads us to our next struggle…
Recruitment challenges revealed
Mrs Evison says that the north-east struggles with this as “the pool of people we can recruit from” is “some distance away”.
“Most of the population of Scotland live in the central belt,” she told the meeting.
So bosses are now increasing efforts to recruit personnel from within the region.
They say this has already had some success, with a “Wish You Worked Here” scheme in Moray proving a hit.
People getting sicker at time of crisis for NHS in north-east
Another reason for the malaise is, quite simply, that people are living longer – and experiencing all of the health complications that can come with that.
But age isn’t the only issue contributing to poor health.
There is an increasing gap between the rich and poor when it comes to wellbeing.

People in deprived areas are suffering from worse health than their wealthier counterparts.
And one fifth of children in the Grampian area are now living in poverty.
“This picture is worsening over time,” the chairwoman warned.
Why are we waiting?
The issue of long waiting times is exasperating patients and their families across the north-east.
And there appears no easy answer to the dilemma.
In Grampian, only 90.8% of people met the “32-day standard” between diagnosis and treatment for cancer beginning across 2023/24, compared to 95.2% the year prior.
At emergency departments, 61.4% of people were treated within four hours – a slight decline from the prior 62.9%.
Mrs Evison said the “deteriorating” position shows a “mismatch between rising demand and capacity to meet that demand”.
There were 166 delayed discharges, up from 75.
What do you think should be done about the healthcare crisis? Let us know in our comments section below
‘This is not what we want to provide’
Summing up, Mrs Evison said: “This performance is not what anyone wants to provide for our population.
“Behind the figures are individuals and their families, we need to do more to fundamentally transform our health system.”
But offering a glimmer of hope, she turned to projects that may once have sounded like something from a futuristic sci-fi movie.
The chairwoman hailed recent projects like deploying drones to deliver vital medication and advances in using artificial intelligence to speed up breast cancer diagnoses.
Read more:
Torphins mum forced to give new-born baby CPR during ‘frightening’ long wait for ambulance
Exclusive: No ambulances available to send to tragic Balmedie toddler due to five-hour queues at ARI






Conversation