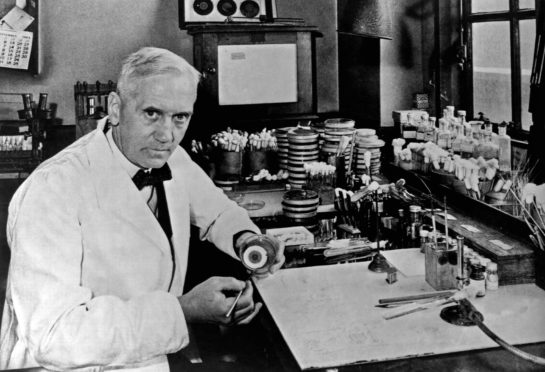
It is just over 90 years since one of Scotland’s most famous sons stumbled on a substance he called “mould juice” and set the world on the path to a medical revolution.
No sooner though had Sir Alexander Fleming discovered penicillin, he found that bugs started to mutate to develop resistance, so the antibiotic would no longer work.
So we started discovering and making different antibiotics, and the bugs developed resistance to them too.
Now we are running out of new antibiotics. Studies across the world show a direct relationship to the number of antibiotics prescribed with the rates of resistance and emergence of superbugs.
Now I’m sure you think global warming and plastics in the ocean are huge problems for our world, but do you think this question of antimicrobial resistance is a one too?
The World Health Organisation certainly does. It calls it a threat to the very core of modern medicine, worse than terrorism or Ebola and predictions are that it will cause more deaths than cancer by 2050.
This is World Antibiotics Awareness Week (#WAAW2019). But are these awareness days and apocalyptic warnings making any difference, or have we all just put our fingers in our ears and decided that it is someone else’s problem, in some other country, sometime in the future?
Because it’s not, it’s a problem now, here in Scotland; when a child is getting treatment for leukaemia, or a young woman has a urinary infection that’s not responding to antibiotics, or your granny picks up a ‘Superbug’ after a hip replacement.
Antimicrobial Resistance is directly related to antibiotic prescriptions.
The good news is that we GPs have reduced our prescribing of them by over 10% in the past five years.
Family doctors in the Highlands have done particularly well. However that still leaves over a quarter of people in Scotland taking at least one course of antibiotic every year. Our new target is to reduce antibiotic prescriptions by a further 15% in the next five years. Scandinavia and The Netherlands have done it already, with no increased problems or deaths from infections, so we can do it too. But we need your help – and there are a number of things we can all do to help the cause.
One is washing our hands regularly – not just after using the toilet but after coughing and sneezing too, preventing colds and flu from spreading.
Another is looking after ourselves – we will be less susceptible to infection if we eat well, exercise more, drink less and don’t smoke.
Checking the need for antibiotics with a community pharmacist or via reliable online sources such as www.treatyourselfbetter.co.uk, www.nhsinform.co.uk or www.patient.info.co.uk can also help. For instance green phlegm is the body’s own defences clearing infection and usually doesn’t need antibiotics. The advice includes warning signs to look out for when medical attention is needed.
Other useful actions include having the flu jab and pneumonia jab if you are at risk, over 65 or work with the public and to consult community pharmacists as many have had extra training in treating minor ailments such as urinary tract infection.
Most patients also now know that antibiotics are not needed for most coughs, earaches and sore throats. Less well known is the change of guidance to using shorter courses for most infections.
So for a woman with a urinary infection, three days is enough, and for respiratory infections such as cough, bronchitis, most sore throats and even pneumonia, five days is all that is needed.
Doctors have been trained for years to give the traditional seven day course, so this new guidance is a big change for us. It’s worth discussing a shorter course with your GP – you could politely point them to the NICE clinical guideline summaries.
It may be that you still have some symptoms such as cough and phlegm after the course is finished, but this is usually residual irritation and taking more antibiotics will not clear these symptoms up any faster.
Local research also shows an increasing amount of pharmaceuticals are also getting into our lovely clean Highland rivers and lochs. Every time we take a medicine it gets excreted in our urine into the local waste water system. It’s a particular concern with antibiotics, when even a minuscule concentration of antibiotic getting into our water supply can encourage hardy, resistant bacteria to swap its genetic material if it mixes with microbes in the bottom sludge of a river -a fast track to developing resistance. So the more antibiotics we take, the more we pass out into the sewage systems that water purification systems are not designed to deal with. Even worse is if we throw unused antibiotics into our bins where they end up in landfill, or flush them down the toilet. Reducing the number of antibiotic prescriptions and taking shorter courses will help, but please take all unused medicines back to the chemist.
We understand the dangers of passive smoking, compromising the health of others. Perhaps we can think of unnecessary antibiotics in the same way? No one needs to smoke, but sometimes people do really need antibiotics. One day you or your loved ones may need treatment – we just want to make sure your antibiotics work for you. Let’s all #KeepAntibioticsWorking
Dr Gail Haddock is a Highland GP, member of Highland Antimicrobial Management Team and Vice Chair of the Scottish Antimicrobial Prescribing Team