The rising number of drug related deaths in Scotland has been extremely difficult for everyone, particularly those affected and those who work in drug and alcohol services.
Increasingly we are seeing deaths linked to “street benzos” or illicit benzodiazepines, which are unpredictable and unlicensed, meaning they often contain varying levels of dangerous substances and can also be mixed with additional unknown substances. In particular it has been very worrying to see young people use these drugs which are cheap and readily available.
The last year has been unquestionably difficult for everyone in Scotland. However, the isolation and additional barriers created for people with a drug dependency dramatically increased when the pandemic began.
Many support services had to drastically reduce provisions in an attempt to keep staff and people accessing services safe. Undoubtedly this resulted in increased isolation, mental health issues and a deterioration of physical health for many who were already struggling to cope.
Unfortunately isolation and poor mental health can lead to substance use and many who have struggled through these challenging times will have used drugs or alcohol in an attempt to cope with the difficulties suddenly thrown at them.
Substance abuse increased in lockdown – but support services adapted
For those in recovery, opportunities for meeting up with familiar faces in support groups, relaxing in meditation classes and regular contact with support networks were ripped away when lockdown began. This sadly led to more people using substances again as a way to fill this void.
Nonetheless, a major positive throughout lockdown has been seeing how services have pulled together and worked collaboratively to ensure vital support still reached those who needed it. Many third sector and NHS services came together immediately to implement new ways of working and innovative practices that will no doubt continue.
Hillcrest Future’s Tayside Injecting Equipment Provision (IEP) Harm Reduction Service in particular managed to remain open to members of the public throughout lockdown, providing a vital face-to-face service for all who needed it.
With the shift to remote support and telephone-based contact, those who have no access to amenities we all take for granted, such as computers, internet or even a phone, were immediately disadvantaged. Many services recognised this and provided mobile phones to allow access to health based appointments, as well as adapting their service delivery so that more outreach based support could take place.
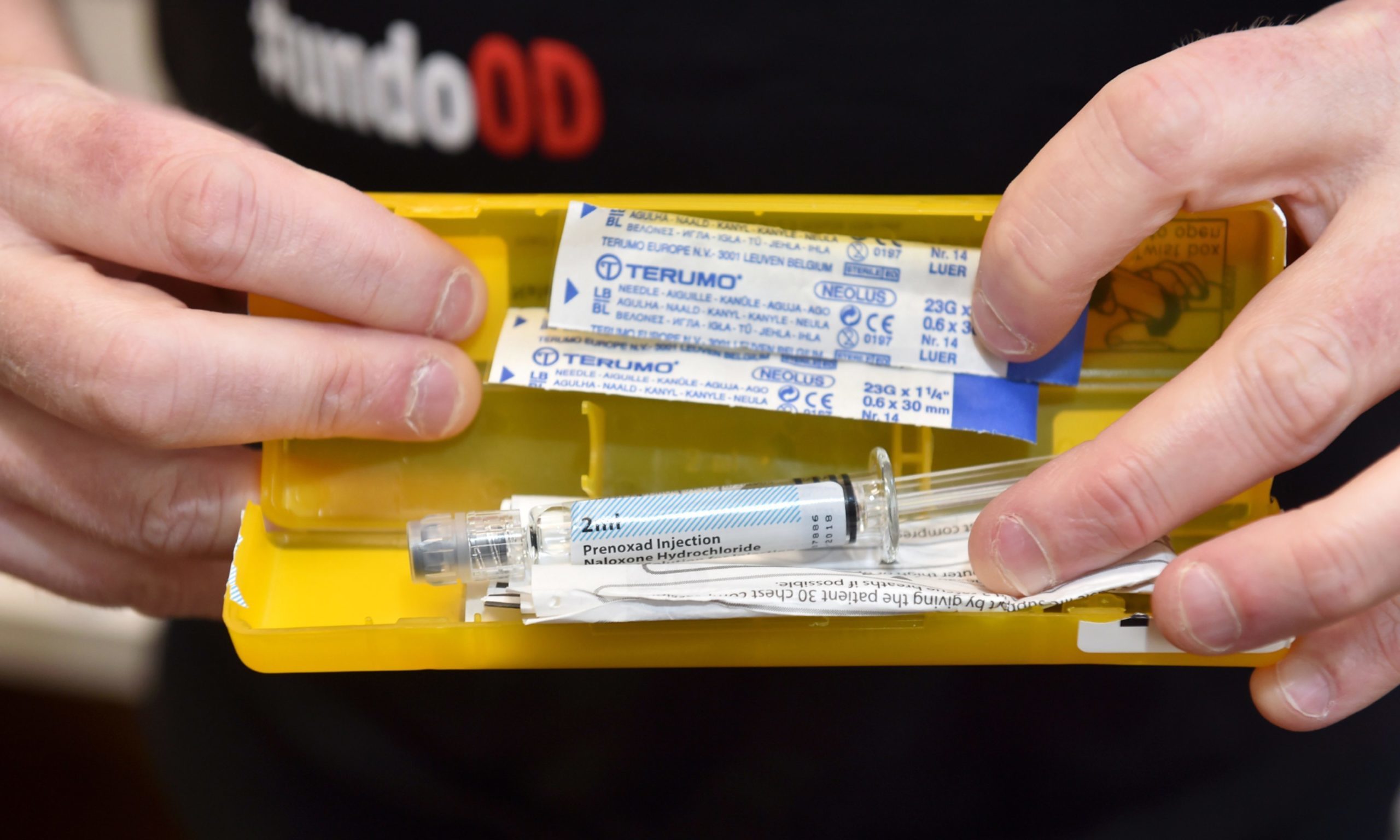
Postal services were created to ensure the life-saving medication naloxone could still be delivered to those who could not leave their home due to the stay at home rules or because of self-isolation and shielding.
Judgement is detrimental to fixing our drug problem
The key message about overdose is that it is entirely preventable. The use of naloxone can reverse the symptoms of overdose and anyone can be trained to use it and provided with a free supply. We need a community response to tackle substance use – to help people not judge and to encourage people to carry naloxone.
Most of the people that I have supported during my four years working in harm reduction consumed their first drug as a child, so it was certainly not an informed choice
Reducing stigma associated with substance use is essential in reducing preventable drug-related deaths. The issue of stigma and the extreme judgement that people with drug dependencies face from society and, unfortunately, from some services ultimately prevents people from seeking support.
It’s easy to assume that all drug use is a choice and therefore that choice should determine how you are treated. However most of the people that I have supported during my four years working in harm reduction consumed their first drug as a child, so it was certainly not an informed choice.
We must align mental health and drug services
No one chooses to create a crippling addiction for themselves. As human beings we are complex creatures with complex emotions and needs.
We already know that substance use can stem from trauma and that using substances more often than not leads to further trauma, so it becomes a devastating cycle to be trapped in until that trauma can begin to be healed.
Aligning mental health services with drug and alcohol services is key to allowing people the opportunity to break free from this trap. Too often mental health support is not available until the drug problem has been resolved. This simply isn’t realistic.
As we all emerge from lockdown – where the whole world has been mildly traumatised – we must now shift our focus to the healing of everyone, including those who were already on a cliff edge of despair before the pandemic made it even harder to cling on.
Fiona Holt is Harm Reduction Coordinator at Hillcrest Futures, a support service based in Dundee